Colon cancer is one of the most common malignancies worldwide, and for many individuals, hearing about its prevalence can spark a great deal of anxiety—especially if you’ve recently experienced concerning gastrointestinal (GI) symptoms. You may notice changes in your bowel habits, unexplained bleeding, or persistent bloating and wonder, “Could it be colon cancer?” The reality is that while some GI symptoms do overlap with colon cancer, they often result from more benign issues such as hemorrhoids, irritable bowel syndrome (IBS), or simple dietary changes.
In this post, we’ll explore the nuances of colon cancer’s early indicators, discuss how they can blend in with other GI problems, and review key screening tests. We’ll talk about why early detection and self-advocacy matter so much—whether you’re a patient worried about that lingering symptom or a caregiver supporting someone through a health scare. By the end, you’ll have a more detailed picture of how to recognize possible warning signs, how to differentiate them from other conditions, and what steps to take for further evaluation. We’ll also share some real-life stories that illustrate the importance of early consultation and testing, as well as practical tips on staying calm and proactive when health concerns arise.
What Is Colon Cancer and Why Awareness Matters
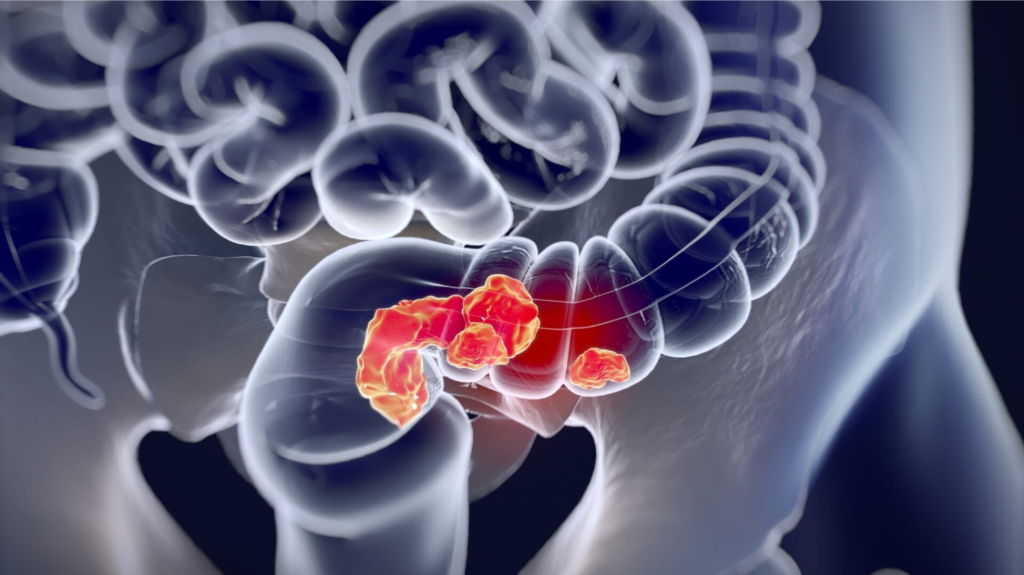
Colon cancer, also called colorectal cancer when it includes the rectum, develops in the large intestine. Polyps—small growths that can form on the lining of the colon—sometimes become cancerous over time. Although not all polyps are malignant, their presence can raise the likelihood of developing colon cancer. Some grow slowly and remain asymptomatic for years, while others may cause noticeable changes in bowel habits or bleeding.
Colon cancer often remains silent until it progresses to a more advanced stage, where treatment may become more complicated. The American Cancer Society and other reputable organizations consistently emphasize that early-stage detection greatly increases the chance of successful treatment. Recent statistics have also led experts to start recommending routine screenings earlier, typically beginning at age 45 for average-risk individuals. If you have a family history or other risk factors, you may need even earlier or more frequent checks.
Raising awareness means helping people differentiate between benign GI issues and more serious signs, ensuring that those who need further evaluation don’t delay it. Often, it can be difficult to know whether new or persistent GI discomfort is worth a medical consult. Learning about common warning signals and how they can overlap with everyday digestive problems is therefore an essential first step in deciding when it’s time to seek help.
Overlapping Symptoms: Why It’s Often Confusing
A big challenge in recognizing colon cancer stems from the fact that its early symptoms frequently mimic other GI conditions. This overlap is one of the primary reasons colon cancer can go undetected or be misdiagnosed, especially in the beginning stages when the disease is easiest to treat. Below are some common GI issues that often blur the diagnostic lines:
Hemorrhoids. Many adults develop hemorrhoids due to prolonged sitting, straining during bowel movements, or other factors that increase pressure in the veins around the anus. Hemorrhoids often cause bright red blood on toilet paper or in the toilet bowl. Understandably, seeing blood can be alarming, yet hemorrhoids remain a very common—and typically less serious—explanation for rectal bleeding.
Anal Fissures. These are small tears in the lining of the anus and can be caused by constipation, passing large or hard stools, or anal trauma. Similar to hemorrhoids, fissures may lead to bright red bleeding and pain during bowel movements, closely resembling symptoms that might otherwise raise concerns about colon cancer.
Irritable Bowel Syndrome (IBS). Characterized by bouts of diarrhea, constipation, or a mix of both, IBS frequently causes abdominal pain and discomfort. Stress, diet, or hormonal changes can trigger flare-ups. Since IBS can produce some of the same discomfort and changes in bowel movements seen in early-stage colon cancer, it’s no surprise that individuals often mistake IBS symptoms for something more ominous—or vice versa.
Inflammatory Bowel Diseases (IBD). Conditions like Crohn’s disease and ulcerative colitis can involve chronic inflammation of the GI tract, leading to pain, diarrhea, and even blood in the stool. Many who have IBD experience periods of remission and flare-ups. This pattern can mask the presence of colon polyps or other potentially malignant changes if one assumes these symptoms are “just another flare.”
Dietary Issues and Stress. Everyday factors—such as food intolerances (lactose, gluten) or high-stress periods—can make your GI system more sensitive. Temporary shifts in bowel habits, mild bloating, or occasional cramps are often attributed to something as simple as a stressful week at work or trying out a new diet.
Because so many GI symptoms are common in daily life, it’s easy to adopt a “wait and see” approach. Sometimes that does work out if the root cause is short-lived—like a minor infection or one-time dietary mistake. However, if symptoms persist or intensify, it’s best to speak to a healthcare provider rather than wait, especially if you have other risk factors like a family history of colon cancer or are over 45.
Risk Factors and Red Flags
Before diving into specific warning signs, let’s briefly talk about risk factors. While anyone can develop colon cancer, certain factors can increase your susceptibility, such as:
- Age 45 or older (screenings have been updated to start earlier).
- Family history of colon cancer or advanced polyps, particularly in first-degree relatives (parents, siblings, children).
- A personal history of IBD, such as Crohn’s disease or ulcerative colitis, which can lead to chronic inflammation in the colon.
- Genetic syndromes like Lynch syndrome or familial adenomatous polyposis (FAP), which significantly raise the likelihood of colon cancer.
- Lifestyle factors including a diet high in red or processed meats, smoking, heavy alcohol use, and physical inactivity.
Just because you have one or more risk factors doesn’t mean you’ll definitely develop colon cancer. However, you may need more vigilant screening or earlier discussions with your healthcare provider about any GI issues that come up.
Key Warning Signs: From Subtle to Serious
In general, the most concerning symptoms of potential colon cancer fall into a few main categories, though they vary in intensity. Below are the broad categories, followed by deeper discussion of how they can differ from other conditions.
1. Changes in Bowel Habits
Prolonged diarrhea or constipation, especially for several weeks or longer, can point to something beyond everyday GI upset. Some people notice that their stools become narrowed or ribbon-like, indicating a potential constriction or obstruction in the colon. IBS often features fluctuating bowel habits that respond to stress management or dietary tweaks. If you’ve made lifestyle adjustments without seeing improvement—or your stools become consistently narrow—it’s time to talk to a healthcare provider.
2. Rectal Bleeding or Blood in the Stool
Blood can appear bright red or cause the stool to look dark or tarry (a sign the blood originated in the upper GI tract). While hemorrhoids, fissures, and even certain foods can influence stool color, persistent or recurring bleeding that doesn’t clear up quickly is a red flag. Seeing darker-colored blood is especially noteworthy and warrants medical attention.
3. Unexplained Weight Loss and Persistent Fatigue
Many people lose or gain a few pounds due to stress, minor infections, or changes in routine. However, losing 5–10% of body weight over six months without deliberate diet or exercise modifications—especially when combined with fatigue—can indicate a deeper issue. Thyroid disorders, chronic infections, depression, and other conditions also explain weight loss, but if none of these apply and you feel unusually tired day after day, don’t ignore the possibility of a GI cause like colon cancer.
4. Abdominal Discomfort or Pain
Cramping, gas pains, or bloating that doesn’t respond to over-the-counter remedies or dietary changes could signal an underlying problem in your intestines. Food intolerances and IBS might produce similar discomfort, but the difference usually lies in severity and duration. If the pain is intense, continuous, or disrupts sleep or daily activities, further evaluation is critical.
5. Feeling Like Your Bowel Doesn’t Empty Completely
A sense of incomplete evacuation can occasionally happen with IBS or insufficient fiber intake, but in some cases, it’s a sign that something is physically or functionally preventing the colon from emptying fully. When combined with rectal bleeding, chronic fatigue, or other unexplained symptoms, it may point to a more serious concern.
Again, experiencing just one of these problems isn’t a guarantee of colon cancer. The key indicator is persistence. If symptoms linger, worsen, or appear alongside other suspicious changes, seeking professional advice is always the safest course of action.
The Emotional Toll of Uncertain GI Symptoms
It’s easy to focus strictly on the medical aspects, but the emotional burden of unexplained GI symptoms can also be significant. Patients and caregivers alike often wrestle with anxiety, worry, or even fear about what these symptoms might mean. The mind may race with worst-case scenarios, and some people delay seeing a doctor because they’re overwhelmed by the idea of a potential cancer diagnosis.
Caregivers, too, can feel this strain, especially if they’re urging a loved one to get evaluated while also trying to provide reassurance. The combination of uncertainty and a barrage of information—much of it found online—can lead to confusion or panic. During these times, it’s helpful to remember that colon cancer is just one possibility, and many GI symptoms turn out to be non-cancerous. Staying informed, maintaining open communication with healthcare providers, and using reputable resources can help reduce the emotional toll.
Critical Tests for Ruling In or Out Colon Cancer
If you’ve decided to see a healthcare provider about your GI symptoms—or you’re encouraging someone else to do so—you’ll likely hear about several screening and diagnostic procedures. Below is an overview of the main tests, with insight into how they work and what results they can yield:
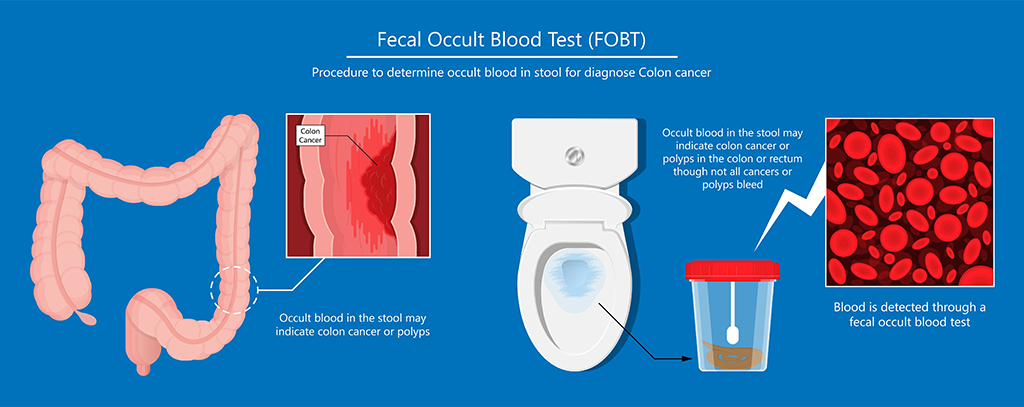
Fecal Occult Blood Test (FOBT) or Fecal Immunochemical Test (FIT).
These tests check for microscopic traces of blood in the stool that might not be visible to the naked eye. You’ll generally receive a kit for at-home stool collection. If the test comes back positive, it indicates bleeding in the GI tract but doesn’t confirm its source. Further evaluation, such as a colonoscopy, is often the next step.
Colonoscopy.
Widely regarded as the gold standard in colon cancer screening, colonoscopy involves inserting a long, flexible tube fitted with a camera into the rectum to examine the entire colon. After completing a bowel-cleansing prep to clear the colon, a specialist can spot and remove suspicious polyps or perform biopsies right away. While the idea of a colonoscopy can be intimidating, it’s an incredibly effective diagnostic tool and can detect even small lesions.
Sigmoidoscopy.
Similar to a colonoscopy but focuses on the sigmoid colon and rectum. This limited view can still detect abnormalities in the lower part of the colon, though if suspicious areas turn up, a full colonoscopy may be necessary later.
CT Colonography (Virtual Colonoscopy).
For those who prefer a less invasive initial screening, CT colonography uses computerized tomography (CT) scans to create a three-dimensional model of the colon. While it’s less invasive than a standard colonoscopy, any suspicious findings typically still require a conventional colonoscopy so that tissue can be sampled or polyps removed.
Blood Tests (CEA).
The carcinoembryonic antigen (CEA) blood test measures levels of a protein that can be elevated in colon cancer. However, many factors can influence CEA, so doctors primarily use it to monitor patients who already have a known cancer diagnosis.
Each of these tests helps distinguish between benign conditions—like hemorrhoids, IBS, or fissures—and more serious possibilities. The conversation with your doctor about which test to undergo often depends on age, personal risk, and family history. If something potentially harmful is discovered, catching it early can make a major difference in treatment outcomes.
Understanding Colon Cancer Staging
When colon cancer is diagnosed, doctors determine its stage to guide treatment. Staging reflects how far the cancer has spread:
- Stage I often indicates that cancer is only in the lining of the colon.
- Stage II may mean it’s grown into or through the wall of the colon but hasn’t yet spread to nearby lymph nodes.
- Stage III suggests it has reached lymph nodes but not distant sites.
- Stage IV indicates the cancer has spread (metastasized) to other organs like the liver or lungs.
Identifying the stage is crucial: early-stage colon cancer (Stages I and II) is more likely to be addressed successfully with surgery alone, while advanced stages often require additional treatments such as chemotherapy or targeted therapies. Early detection frequently translates to more effective and less extensive treatment plans.
Two Real-Life Stories: Why Early Testing Matters
Case 1: Alarming Symptoms but No Cancer
Karen, a 48-year-old mother of two, started noticing bright-red bleeding during bowel movements and experienced a week of intense cramping. Worried it could be colon cancer, she scheduled an immediate appointment. An initial fecal occult blood test came back positive, so she proceeded with a colonoscopy. While she was anxious about the possibility of cancer, her colonoscopy revealed severe hemorrhoids and a small anal fissure—painful but treatable conditions with no malignant findings.
The relief Karen felt was immense. By seeking help right away, she learned that her symptoms, although scary, were not due to cancer. She also received prompt treatment for her hemorrhoids and fissure, significantly improving her comfort and quality of life. Karen’s experience underscores that concerning symptoms don’t always mean the worst-case scenario. However, her decision to consult a doctor immediately let her rule out more serious causes and begin effective treatment.
Case 2: Mild Symptoms, Advanced Colon Cancer
Robert, a 52-year-old accountant, had a very different experience. Over several months, he felt as though he needed to use the restroom more often, and sometimes his stools were narrower than usual. Because he wasn’t experiencing severe pain or obvious bleeding, he attributed these changes to stress at work. Robert’s wife urged him to see a doctor, but he kept putting it off.
During a routine check-up, Robert casually mentioned his bowel changes. His physician recommended a Fecal Immunochemical Test (FIT), which came back positive for hidden blood. A follow-up colonoscopy revealed a sizable tumor in his transverse colon. By the time he was diagnosed, the cancer had progressed to a stage that required not only surgery but also chemotherapy. Robert’s case illustrates how subtle symptoms can sometimes indicate serious disease. An earlier evaluation could have led to a Stage I or II discovery, giving him more straightforward treatment options and potentially better outcomes.
How to Advocate for Yourself or a Loved One
In both Karen’s and Robert’s stories, the importance of timely medical attention is crystal clear. Whether you’re the patient or the caregiver, self-advocacy and awareness can be life-changing. Here are strategies that can help:
Speak Up Early and Often. Even minor symptoms can have major implications if they persist. Talk openly with healthcare professionals about what you’re experiencing, how long it’s lasted, and what interventions you’ve tried.
Know Your Risks. If you’re age 45 or older, have a family history of colon cancer, or have chronic conditions like IBD, discuss screening guidelines with your provider. Early and regular screenings can catch cancer in its infancy or identify pre-cancerous polyps.
Seek a Second Opinion. Never hesitate to seek another viewpoint, especially if your symptoms continue without improvement or if you feel your concerns aren’t being taken seriously. Specialists like gastroenterologists or colorectal surgeons can offer deeper insight if you’re uncertain about a diagnosis.
Keep a Symptom Diary. Track your bowel movements, energy levels, dietary changes, and any new or intensified symptoms. This record offers valuable data for your physician, helping them determine patterns or triggers.
Lifestyle Adjustments. While not a guarantee against colon cancer, healthy habits can lower the odds. A diet high in fiber, fruits, and vegetables, combined with limiting red or processed meats, regular exercise, and quitting smoking, has been linked to reduced risk.
Rely on Reputable Sources. Misinformation can create unnecessary fear or cause dangerous delays in seeking care. Trustworthy organizations like the American Cancer Society, National Cancer Institute, and Mayo Clinic offer evidence-based guidance on colon cancer.
Practical Tips for Handling Worry and Next Steps
Stay Calm but Alert. GI issues like a single bout of constipation or one episode of spotting in the stool are common and may resolve spontaneously. Nevertheless, pay attention to repeated occurrences.
Prepare for Your Appointments. Write down your questions, concerns, and any relevant family history to ensure your time with the physician is used effectively. Arrive ready to discuss what has been happening and for how long.
Follow Medical Instructions Thoroughly. If you’ve scheduled a colonoscopy, strictly adhere to the bowel-prep guidelines. Though sometimes inconvenient, proper prep ensures your doctor has the clearest possible view. This greatly boosts the accuracy and safety of the procedure.
Consider Sedation Options. Colonoscopies can be done with sedation or anesthesia to minimize discomfort and anxiety. If you’re worried about pain or feeling embarrassed, ask about sedation that will help you remain relaxed or even sleep through the procedure.
Build a Support System. Whether you’re the one experiencing symptoms or supporting someone else, it helps to have a loved one accompany you to appointments, take notes, or help you follow post-procedure instructions. Emotional support can be as vital as the medical care itself.
Additional Considerations for Caregivers
Caregivers play a pivotal role when someone close to them faces uncertain GI symptoms. In addition to emotional support, caregivers often help schedule appointments, drive patients to and from procedures (especially if sedation is involved), and manage day-to-day tasks that become challenging if the patient is in discomfort or undergoing treatments. Communication is vital: encourage the person you’re caring for to share their fears or questions, and if you can, join them during consultations to help recall important details and instructions.
Also, don’t forget your own well-being. Caregiving can be emotionally and physically draining, particularly when the possibility of a cancer diagnosis looms. Seek out support groups, online communities, or counseling if you’re feeling overwhelmed. Balancing your loved one’s needs with your own health is important for both of you.
The Importance of Early Detection
Colon cancer’s warning signs can be subtle, mirroring many other GI conditions. This overlap can lead individuals to either downplay symptoms or assume the worst without proper evaluation. Karen’s story offers reassurance that alarming symptoms can turn out to be non-cancerous, while Robert’s experience is a cautionary tale about delaying a check-up for what seemed like minor changes. The common thread is that seeing a doctor early provides clarity. If symptoms are benign, you’ll likely find relief and a straightforward treatment plan. If they point to something more serious, early detection often means simpler, more successful intervention.
For many, fear or embarrassment acts as a barrier to scheduling appointments. However, addressing symptoms head-on usually reduces overall anxiety. Even if a colonoscopy or other procedure detects polyps, removing them at an early stage can prevent future malignancies. And if colon cancer is found, catching it when it’s still confined to a small area can vastly improve treatment outcomes.
Conclusion
Navigating GI symptoms can feel daunting, especially when the term “colon cancer” enters the conversation. Yet knowledge truly is power. Recognizing the common overlaps between colon cancer symptoms and those of hemorrhoids, IBS, or dietary issues helps you gauge the potential seriousness of what you’re experiencing. Watching for persistent or worsening changes is the key to deciding when to seek professional advice.
If you’re worried or uncertain, remind yourself that not all GI symptoms signal cancer—but they shouldn’t always be dismissed out of hand, either. By speaking with a healthcare provider, undergoing appropriate tests, and advocating for yourself if something feels off, you’ll take proactive steps toward safeguarding your health. As both Karen and Robert’s stories reveal, timely checks can either bring relief or initiate earlier treatments, both of which are far better outcomes than living in prolonged doubt.
Finally, if you’re a caregiver, remember that your role is multifaceted. Offering emotional support is crucial, but so is encouraging your loved one to follow through on medical evaluations. Together, you can overcome the fear and confusion that often accompany uncertain GI symptoms. With patience, vigilance, and supportive care, you’ll be better prepared to deal with whatever the diagnosis may be—and hopefully ensure that, if it is colon cancer, it’s caught at the earliest possible stage.
Sources
Disclaimer: This post is for informational purposes only and does not substitute professional medical advice. Always consult a qualified healthcare provider for personalized guidance regarding any medical condition.


