Circulating tumor DNA (ctDNA) and minimal residual disease (MRD) testing are rapidly transforming the landscape of cancer care. By offering a noninvasive window into the molecular status of a patient’s disease, these technologies are enabling earlier detection of recurrence, more precise monitoring of treatment response, and increasingly personalized therapeutic strategies. However, as with any emerging technology, ctDNA/MRD testing comes with both significant benefits and important limitations. This post explores the science, clinical applications, common tests, and misconceptions surrounding ctDNA/MRD in oncology.

What Are ctDNA and MRD?
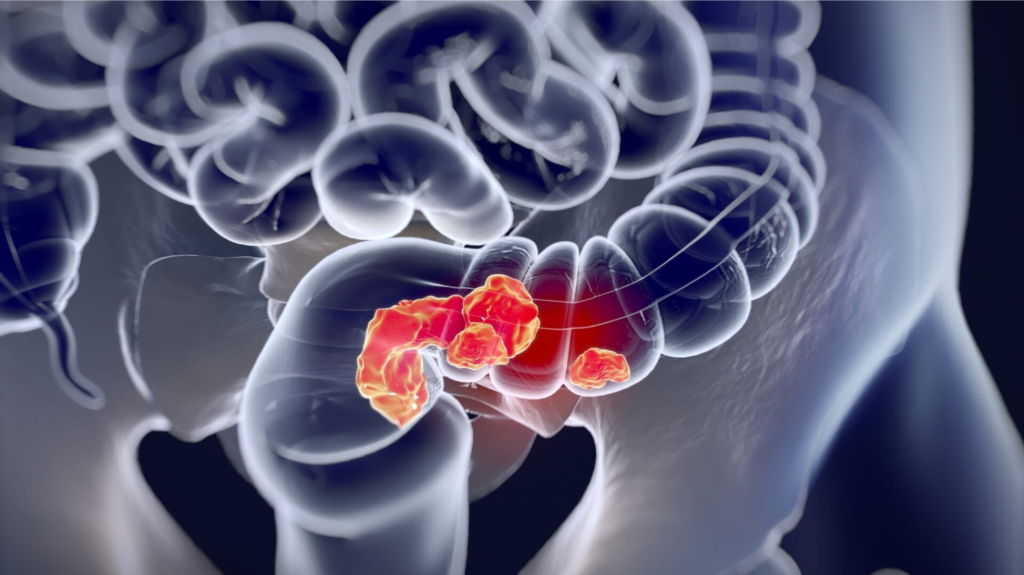
ctDNA refers to fragments of DNA shed by tumor cells into the bloodstream. These fragments can be detected and analyzed through a simple blood draw, often called a “liquid biopsy.” Because ctDNA carries tumor-specific genetic alterations, its presence and quantity can provide real-time insights into tumor burden and behavior86.
Minimal Residual Disease (MRD) describes the small number of cancer cells that may remain in the body after treatment, even when imaging or other tests suggest remission. MRD is a major source of relapse and metastasis in many cancers36. Detecting MRD early is crucial for timely intervention and improved outcomes.
How Are ctDNA/MRD Tests Used in Cancer Care?
Key clinical applications of ctDNA/MRD tests include:
Early Detection of Recurrence: ctDNA/MRD tests can identify molecular relapse months before clinical or radiological evidence appears, allowing for earlier intervention156.
Monitoring Treatment Response: Changes in ctDNA levels during or after therapy can indicate how well a patient is responding, sometimes more sensitively than imaging or traditional biomarkers68.
Guiding Adjuvant Therapy: MRD-positive patients after surgery or initial therapy may benefit from additional (adjuvant) treatment, while MRD-negative patients might avoid unnecessary toxicity58.
Personalized Therapy Selection: ctDNA analysis can reveal actionable mutations, guiding targeted therapy choices when tissue biopsies are not feasible8.
Resistance Genotyping: ctDNA can detect emerging resistance mutations, helping clinicians adjust therapies in real time68.

Common ctDNA/MRD Tests and Technologies
Several ctDNA/MRD assays are now available or in advanced development, each with unique features:
| Test/Platform | Approach | Typical Indications |
|---|---|---|
| Signatera™ (Natera) | Tumor-informed, personalized NGS | MRD detection in colorectal, lung, and other solid tumors post-surgery |
| Guardant Reveal™ | Tumor-naïve, targeted NGS | MRD detection in colorectal cancer, therapy monitoring |
| FoundationOne Liquid CDx | Tumor-naïve, broad NGS panel | Molecular profiling, therapy selection, some MRD applications |
| CAPP-Seq | Tumor-informed, hybrid capture NGS | MRD in lung and other cancers, research use |
| MRDetect | Tumor-informed, WGS-based | Early-stage NSCLC MRD detection, research use5 |
- Tumor-informed assays are customized for each patient using mutations identified from their tumor tissue. This increases sensitivity and specificity for MRD detection75.
- Tumor-naïve assays use predefined panels of common mutations, offering faster turnaround but sometimes lower sensitivity for MRD7.
Benefits of ctDNA/MRD Testing
- Noninvasive: Blood-based testing avoids the risks and discomfort of tissue biopsies8.
- Dynamic Monitoring: Enables repeated, real-time assessment of tumor dynamics throughout treatment68.
- Earlier Detection: Can reveal molecular relapse or resistance before clinical symptoms or imaging changes56.
- Personalization: Facilitates tailored therapy based on individual tumor genetics and MRD status8.
- Potential to Spare Overtreatment: MRD-negative patients may avoid unnecessary adjuvant therapy, reducing toxicity and cost8.
Shortcomings and Limitations
Despite its promise, ctDNA/MRD testing faces several challenges:
- Sensitivity and Specificity: Detection limits vary by assay, tumor type, and disease stage. Small tumors or low-shedding cancers may yield false negatives57.
- Clinical Utility Still Evolving: In many scenarios, ctDNA results do not yet change management for most patients. For example, a Mayo Clinic study found that only 16% of ctDNA MRD tests in CRC led to changes in clinical decisions2.
- False Positives/Negatives: Biological and technical factors (e.g., clonal hematopoiesis, assay noise) can confound results, leading to misinterpretation7.
- Standardization Needed: Different assays and protocols complicate result interpretation and cross-study comparisons37.
- Limited Evidence in Some Cancers: Most data come from colorectal and lung cancers; evidence in other tumors is still emerging68.
Common Misunderstandings About ctDNA/MRD Test Results
1. “A Negative ctDNA/MRD Test Means I’m Cured.”
Reality: A negative result greatly reduces the risk of recurrence but does not guarantee cure. Some tumors may not shed enough DNA to be detected, or the test may miss rare mutations57.
2. “A Positive ctDNA/MRD Test Means Recurrence Is Certain.”
Reality: While ctDNA positivity is a strong predictor of relapse, not all patients with detectable ctDNA will clinically relapse. Some may clear their MRD with ongoing therapy, or the detected DNA may not represent viable tumor cells25.
3. “ctDNA/MRD Testing Replaces Imaging or Other Biomarkers.”
Reality: ctDNA is a complementary tool, not a replacement. Imaging, clinical assessment, and traditional biomarkers remain essential for comprehensive cancer care28.
4. “All ctDNA/MRD Tests Are the Same.”
Reality: Assays differ in sensitivity, specificity, and clinical validation. Tumor-informed tests are generally more accurate for MRD but require tumor tissue and longer setup time75.
5. “A Change in ctDNA Always Requires a Change in Treatment.”
Reality: Most ctDNA MRD results do not currently lead to immediate management changes. Decisions should be made in the context of all clinical information and ongoing research23.
Future Directions and Ongoing Research
- Prospective Trials: Large, prospective studies are underway to better define when and how ctDNA/MRD testing should guide therapy.
- Standardization: Efforts are ongoing to harmonize assay methods, reporting, and interpretation guidelines37.
- Expanding Indications: Research is exploring ctDNA/MRD’s role in early detection, screening, and additional cancer types8.
- Integration with Other Modalities: Combining ctDNA with imaging and other biomarkers may further improve accuracy and patient outcomes8.
Conclusion
ctDNA and MRD testing represent a major advance in personalized cancer care, offering earlier, more precise, and less invasive monitoring of disease status. Their greatest strengths lie in detecting recurrence before it is clinically apparent, guiding adjuvant therapy, and tailoring treatment to individual risk. However, these tests are not infallible: their results must be interpreted with caution, in the context of each patient’s unique disease and in conjunction with other clinical data. As the technology matures and evidence grows, ctDNA/MRD testing will likely become an increasingly routine—and indispensable—part of oncology practice865.
“Liquid biopsy or circulating tumor DNA started with advanced next-generation sequencing-based platforms but has now moved into detecting minimal residual disease. This allows us to spare patients the toxicity of unnecessary treatments and focus on those who need it.”
— Dr. Pashtoon Kasi, Medical Oncologist8


Pingback: What to Expect After a Cancer Diagnosis