A diagnosis of advanced, or metastatic, breast cancer can be overwhelming. However, treatments have evolved significantly in the past decade, transforming survival rates and overall quality of life for many patients. Among these advances, targeted therapies stand out as particularly impactful. Unlike traditional chemotherapy, which indiscriminately attacks rapidly dividing cells, targeted therapies aim for precise molecular features of the cancer, often resulting in greater effectiveness and fewer side effects. As a result, many people are experiencing longer survival times and a better day-to-day experience despite a stage IV diagnosis.
In this post, the focus is on how targeted therapies are reshaping the treatment landscape of advanced breast cancer. We will look at how these treatments work, delve into the major subtypes of breast cancer, provide examples of specific drugs, and offer guidance on managing potential side effects. The goal is to make this information as clear and reader-friendly as possible, while still providing the most up-to-date insights for patients and caregivers. It is important to remember that this information is for general education and should never replace personalized medical advice. Always consult a qualified healthcare provider for any decisions about your diagnosis or treatment.
UNDERSTANDING ADVANCED BREAST CANCER
Breast cancer becomes advanced when it spreads, or metastasizes, beyond the breast and nearby lymph nodes to organs like the lungs, liver, bones, or brain. Some individuals present with metastatic disease at the time of diagnosis (stage IV), while others progress to an advanced stage after receiving prior treatments for earlier disease. Although metastatic breast cancer is typically not considered curable, it can often be managed for an extended period, with the goals of prolonging survival, maintaining or improving day-to-day well-being, and controlling symptoms.
A multidisciplinary approach is especially valuable for patients in this situation. Oncologists, surgeons, radiation specialists, palliative care professionals, nutritionists, and counselors each play a role in addressing the physical and emotional challenges of the disease. Historically, chemotherapy was the mainstay for advanced breast cancer; it could be effective in slowing tumor growth, but it also carried significant side effects and often offered only limited remission. Research into the molecular underpinnings of breast cancer has changed that paradigm. By identifying specific “targets” in the tumor, scientists have developed a wide range of targeted therapies, allowing for more precise—and sometimes more powerful—treatment options.
What makes a therapy “targeted”?
Targeted therapies are designed to home in on specific molecules that help cancer cells grow, divide, or survive. By interfering with these precise molecular pathways, these treatments often spare a greater number of healthy cells, which tends to reduce certain side effects. At the same time, the cancer-fighting potential can be higher when the tumor displays the relevant target.
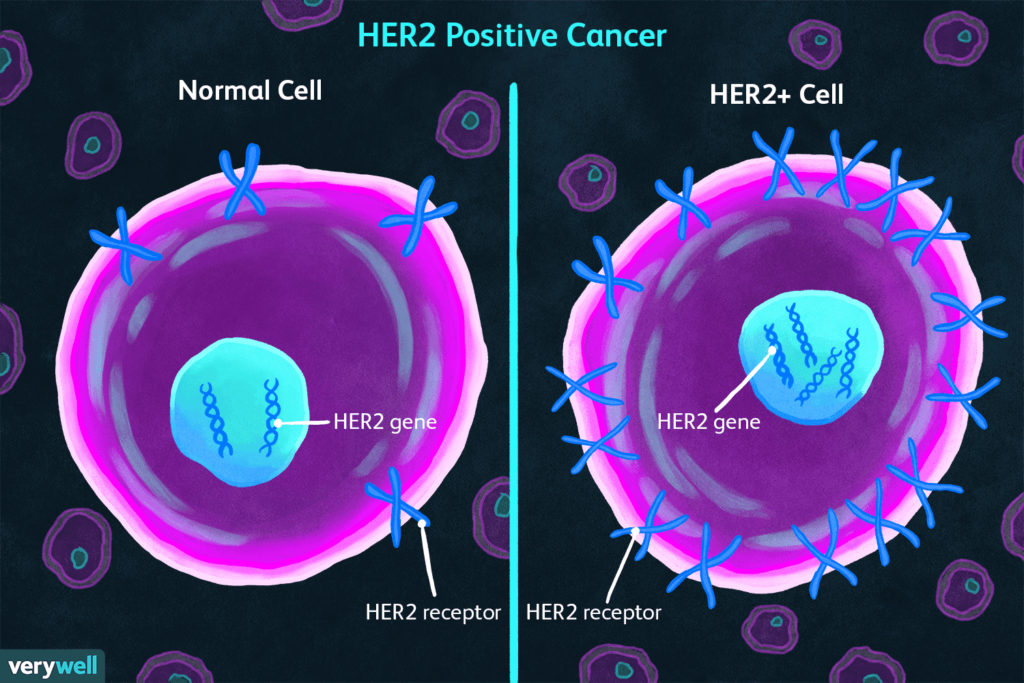
Common targets in advanced breast cancer include HER2 (a growth factor receptor), hormone receptors such as estrogen or progesterone receptors (ER and PR), and mutated genes like BRCA1 or BRCA2. Additional targets involve regulatory pathways within the cells, such as CDK4/6, PI3K, and others. Sometimes multiple targets appear in a single tumor, and treatment approaches must adapt if the cancer evolves or becomes resistant over time.
THERAPY FOR DIFFERENT SUBTYPES OF BREAST CANCER
Breast cancers are typically described based on the presence or absence of three main receptors. Hormone receptor–positive (HR+) tumors carry estrogen (ER) and/or progesterone (PR) receptors. HER2-positive cancers overexpress or amplify the HER2 protein, and triple-negative breast cancer (TNBC) lacks ER, PR, and HER2 expression. Treatment approaches differ substantially across these categories.
For instance, a HER2-positive tumor often responds well to anti-HER2 drugs such as trastuzumab, while hormone receptor–positive disease can be sensitive to endocrine therapies in combination with drugs like CDK4/6 inhibitors. When a tumor is triple-negative, the lack of these receptors can make it more challenging to treat, but researchers have made progress with immunotherapies, PARP inhibitors, and antibody-drug conjugates in selected situations. Understanding a tumor’s specific subtype and molecular profile is pivotal in guiding the choice of therapy.
TARGETED THERAPIES FOR HER2-POSITIVE DISEASE
Approximately 15 to 20 percent of breast cancers overexpress the HER2 receptor, which historically signaled an aggressive form of the disease. The introduction of HER2-targeted treatments changed this outlook drastically.
Drugs like trastuzumab, the first anti-HER2 antibody approved, block HER2-driven growth signals and are frequently used alongside chemotherapy. Pertuzumab was later developed to bind a different area of the HER2 receptor, often leading to even better outcomes when combined with trastuzumab and chemotherapy in the first-line metastatic setting. Other notable therapies include T-DM1 (ado-trastuzumab emtansine), an antibody-drug conjugate that links trastuzumab to a chemotherapy agent, delivering the toxic payload directly to HER2-positive cells. Fam-trastuzumab deruxtecan-nxki (Enhertu) takes this concept further by attaching a powerful chemotherapy to the HER2-targeting antibody, showing remarkable efficacy in patients who have already progressed on multiple other treatments. Oral tyrosine kinase inhibitors, such as lapatinib, target HER2 signaling from inside the cell and can be combined with chemotherapy or hormonal therapies, depending on the patient’s tumor type.
For many individuals with HER2-positive breast cancer, these therapies have turned what was once one of the most aggressive subtypes into a more manageable, long-term condition, dramatically improving both progression-free and overall survival.
TARGETED THERAPIES FOR HORMONE RECEPTOR-POSITIVE (HR+) DISEASE
Breast cancers that rely on hormones like estrogen and progesterone for growth (ER+ and/or PR+) have long been treated with endocrine therapies to block these hormonal pathways. More recently, adding targeted drugs to endocrine therapy has further improved outcomes.
CDK4/6 inhibitors—such as palbociclib, ribociclib, and abemaciclib—are used alongside aromatase inhibitors or the estrogen receptor degrader fulvestrant. By inhibiting key enzymes in the cell cycle, they significantly delay cancer progression and allow many patients to avoid chemotherapy for longer periods. PI3K inhibitors, like alpelisib, target a common mutation (PIK3CA) in HR+ breast cancer cells, and are usually combined with fulvestrant for patients who have previously tried other endocrine therapies. Another class of drugs, mTOR inhibitors (e.g., everolimus), helps overcome resistance to hormone therapies by blocking a growth pathway inside the cancer cells.
A typical example is a patient who starts with an aromatase inhibitor but shows signs of progression. If her tumor has a PIK3CA mutation, the oncologist might add alpelisib plus fulvestrant. If not, a CDK4/6 inhibitor could be another effective choice. By layering targeted agents on top of endocrine therapy, many patients experience a notable extension of disease control with relatively tolerable side effects.
STRATEGIES FOR TRIPLE-NEGATIVE BREAST CANCER (TNBC)
Triple-negative breast cancer does not express ER, PR, or HER2, making it historically resistant to standard targeted or hormonal therapies. Chemotherapy used to be the only option, especially for advanced or metastatic disease, but recent breakthroughs are beginning to alter that landscape.
One important advance involves PARP inhibitors like olaparib or talazoparib for patients who carry BRCA1 or BRCA2 mutations. By blocking a critical DNA repair pathway, these drugs selectively weaken cancer cells that already have compromised DNA repair functions. Another avenue, immunotherapy, shows promise in a subset of triple-negative tumors, particularly those that test positive for the PD-L1 protein. Medications such as atezolizumab and pembrolizumab, which harness the immune system against tumor cells, have improved outcomes when combined with chemotherapy in PD-L1-positive TNBC.
Finally, antibody-drug conjugates (ADCs) have become increasingly relevant for TNBC. Sacituzumab govitecan targets the Trop-2 protein found on many TNBC cells, effectively delivering a potent chemotherapy payload directly to the tumor while minimizing some of the systemic side effects. Although TNBC remains more challenging to treat, these new strategies are gradually improving survival and hope for affected individuals.
MANAGING SIDE EFFECTS
Although targeted therapies often spare healthy cells more effectively than conventional chemotherapy, they can still produce side effects that vary by drug class. Individuals receiving HER2-directed treatments such as trastuzumab and pertuzumab may develop heart-related issues, requiring regular cardiac monitoring. CDK4/6 inhibitors can cause low white blood cell counts and some gastrointestinal discomfort, whereas PI3K inhibitors may contribute to high blood sugar and skin rashes. PARP inhibitors can lead to nausea, fatigue, or anemia, and immunotherapies used in TNBC may trigger immune-related inflammatory conditions like thyroid dysfunction or pneumonitis.
Communication with the healthcare team is vital in these situations. Doctors can adjust doses, recommend supportive medications, or intervene early to keep side effects from becoming severe. Many patients find it useful to keep a diary or symptom journal, track their daily energy levels, and note any physical changes so they can share accurate information with their oncology providers. Lifestyle adjustments—such as staying hydrated, engaging in gentle exercise approved by the care team, and eating a nutritious diet—can also make a noticeable difference in managing symptoms.
PATIENT SCENARIOS AND REAL-WORLD EXPERIENCES
One example involves a patient initially diagnosed with HER2-positive early-stage breast cancer who received surgery, chemotherapy, and adjuvant trastuzumab. Two years later, she develops metastatic lesions in her liver, confirmed to be HER2-positive. Her oncologist may prescribe docetaxel plus trastuzumab and pertuzumab. After a period of strong response, she might transition to maintenance with HER2-targeted therapy alone, often staying stable on this regimen for over a year.
Another scenario is an individual with hormone receptor–positive (ER+/HER2–) metastatic breast cancer who had already received an aromatase inhibitor. Molecular testing shows a PIK3CA mutation, so the oncologist combines fulvestrant with alpelisib. Imaging scans reveal tumor shrinkage, and the patient experiences mostly manageable side effects like mild skin rash and occasional hyperglycemia, carefully overseen by her medical team.
A third case might involve a patient with triple-negative breast cancer who tests positive for the BRCA1 mutation. After failing standard chemotherapy, she moves on to a PARP inhibitor like olaparib. This approach results in stable disease for several months and leads to fewer side effects than her previous treatments, improving her overall sense of well-being.
THE FUTURE OF TARGETED THERAPIES
Targeted therapies are a dynamic and quickly evolving field. Researchers are working on next-generation antibody-drug conjugates (ADCs) targeting proteins like HER3 or Trop-2, building upon the success of T-DM1 and trastuzumab deruxtecan. Combination therapies that merge immune checkpoint inhibitors with CDK4/6 inhibitors, PARP inhibitors, or PI3K inhibitors are under investigation to see if they can prevent or delay resistance. Additionally, scientists are refining biomarker tests to identify those who are most likely to respond well to a given targeted agent. Efforts to develop oral selective estrogen receptor degraders (SERDs) are ongoing, promising a more convenient option than the injectable form. Experimental approaches such as personalized cancer vaccines and CAR T-cells, though still in early phases, hint at the possibility of even more individualized treatments in the years to come.
Patients can stay informed about emerging trials and newly approved drugs by visiting sites like ClinicalTrials.gov or tracking reputable cancer organizations. Regular discussions with a medical team that keeps current on these developments can also open up opportunities to join clinical studies or access innovative treatments.
See more about the latest treatments in metastatic breast cancer HERE
CONCLUSION
Targeted therapies have ushered in a new era of care for advanced breast cancer. In contrast to the older, one-size-fits-all chemotherapy methods, these newer options can offer better disease control with reduced toxicity. HER2-positive tumors, which once carried a particularly poor prognosis, now often respond to a range of sophisticated HER2-targeting drugs. Hormone receptor–positive disease may remain stable for long stretches with the help of CDK4/6 or PI3K inhibitors. Even for triple-negative breast cancer, emerging treatments like immunotherapy, PARP inhibitors, and antibody-drug conjugates are making meaningful inroads.
Living with advanced breast cancer is undoubtedly challenging, both physically and emotionally. However, the expanding pipeline of targeted agents has brought fresh hope and an increased likelihood of longer survival. Working closely with an experienced oncology team, communicating about side effects, and staying engaged with supportive communities can all contribute to a more manageable journey. Even with a stage IV diagnosis, many people are finding ways to maintain a fulfilling life while receiving effective, personalized treatment.
SOURCES:
- BreastCancer.org
- American Society of Clinical Oncology (ASCO)
- National Cancer Institute (NCI)
- European Society for Medical Oncology (ESMO)
- NCCN Clinical Practice Guidelines in Oncology
- ClinicalTrials.gov – Database of current clinical trials
- METAvivor – Organization focused on metastatic breast cancer research and support
Disclaimer: This blog post is for informational purposes only and does not replace professional medical advice. Always consult a qualified healthcare professional regarding any decisions about diagnosis, treatment, or overall management of breast cancer. You are not alone—teams of specialists, patient advocates, and supportive resources stand ready to help navigate each step of your advanced breast cancer journey.



Pingback: CASE SELECTION 3: Long-Term Survival with Advanced Triple-Negative Breast Cancer