Prefer listening? Check out our podcast version!
When you’re living with cancer or caring for someone who is, certain dates start to take on a different meaning. The day of the scan. The day before the scan. The day you receive the results. It’s not just another appointment on the calendar—it’s a countdown, a waiting game, a mental storm. This emotional rollercoaster has a name: scanxiety.
Scanxiety isn’t just about CTs, MRIs, or PET scans. It’s also about waiting for biomarker blood tests, ctDNA monitoring, or tumor markers. It’s the unease that creeps in days before the appointment, the tension of watching the doctor’s face as they read your chart, the overwhelming silence that follows when results are pending.
How Common is Scanxiety?
If you’ve felt scanxiety, know this—you are not alone. In fact, you’re in the majority. Research shows it affects up to 83% of cancer patients at some point during their journey. And caregivers? They’re deeply impacted too.
“I live in a 3-week window. That’s my schedule—blood test every 3 weeks, CT scan every 3 months. I feel light and joyful in the first week after good results, but by week 3, the darkness creeps back. Two nights before my doctor’s visit, I can’t sleep. I’m terrified it’ll be bad news.”
“I used to be the optimist in the family. When my daughter failed a test, I took her on a road trip to remind her of the bigger picture. But now, I spend Sundays glued to my laptop, scrolling through Facebook groups and research papers trying to make sense of why my CEA jumped from 2.5 to 4.7. I miss who I used to be.”
Scanxiety doesn’t stop at the patient. Caregivers often carry a heavy emotional burden, hidden behind brave smiles.
“Since diagnosis, my husband refuses to look at any results. He just trusts the doctors and goes along. I admire that. But every 3 months, I lose my appetite, my sleep, and sometimes my grip. I never show it in front of him—it’s exhausting to carry it all alone.”
Scanxiety isn’t weakness. It’s a shared reality. A deeply human response to uncertainty, especially when so much is at stake.

Will Scanxiety Ever Go Away?
The honest answer? It may not fully disappear. Because cancer, even when stable or in remission, often requires ongoing monitoring. Cancer today is often treated as a chronic condition, but it’s an unpredictable one. No scan, no test, no number can promise the future.
Even after a series of good results, fear can return. Cancer can come back after five, ten, even twenty years. So yes, scanxiety lingers—but its shape can change.
- Persistent but Variable: For some, the anxiety softens over time. Familiarity with procedures helps. But any scan, especially after a scare, can bring it all rushing back.
- Everyone’s Experience is Unique: Younger patients, those with aggressive cancers, or who’ve had previous recurrences may find scanxiety stronger or longer lasting. Others may find new strategies, support systems, or mindsets that help them cope.
- Uncertainty Is the Root: At its heart, scanxiety stems from not knowing. From having lived through a day when everything changed—and fearing it could happen again.
How to Live with Scanxiety
We can’t always eliminate scanxiety. But we can learn to live with it, in a way that’s less overwhelming and more manageable. A helpful way to explore this is through a holistic lens: by tending to our physical, cognitive, social, and emotional well-being.
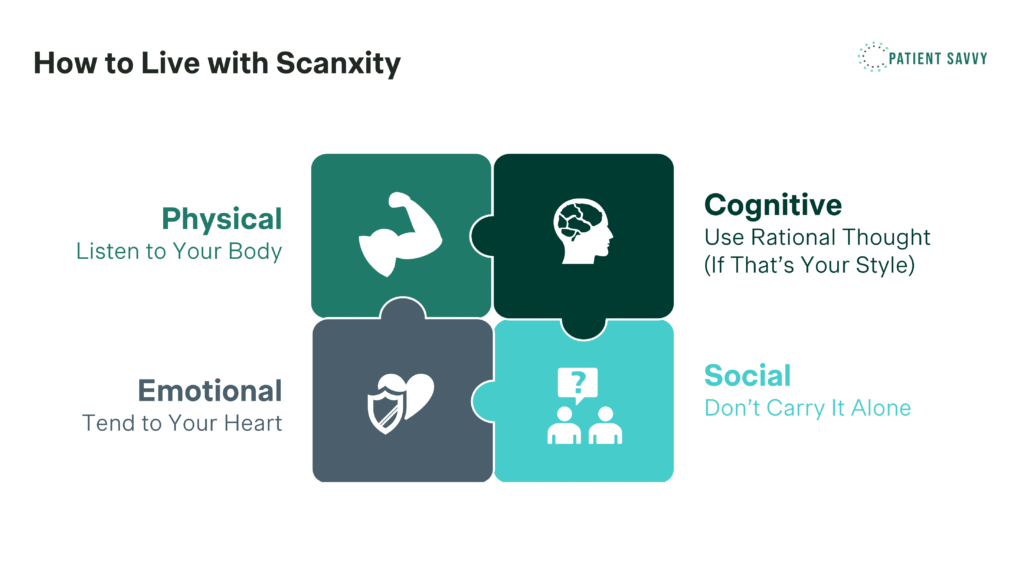
Physical: Listen to Your Body
Test results are just snapshots—a freeze-frame of your condition at a given moment. But you are more than numbers. Pay attention to your own body each day. Are you sleeping okay? Is your appetite changing? Are there new or unusual symptoms? Sometimes, tuning in to these day-to-day experiences can offer a sense of agency, especially when the scans feel out of your control.
If you feel completely healthy—even in the face of a concerning test result—it often means your body is still strong enough to handle what’s ahead, whether that’s another round of treatment or a more invasive procedure. On the other hand, if something feels off in your body, even when your scan appears fine, it’s essential to take those feelings seriously and seek clarity. Your body speaks in more ways than a scan can show.
It’s also important to remember: you can feel healthy and still have a serious diagnosis. These truths are not contradictory. Doing something physical, like gentle stretching, walking outdoors, or even dancing around the kitchen, can ground you in the present and remind you that you’re still here, still moving.
Cognitive: Use Rational Thought (If That’s Your Style)
Not everyone wants to research their condition or dig deep into treatment options, and that’s okay. But for some, having a plan—or at least knowing there’s a plan—can help ease the mental fog of uncertainty. If you’re someone who finds structure calming, try breaking the process into steps: know when your next scan is, understand the potential follow-up options, and talk to your care team about what “next steps” might look like if something changes.
Knowing that many lines of therapy exist might help you feel less cornered. A scan / test result is a chapter—not the whole story.
I’m living with stage IV gastric cancer. Right now, things are under control, but I’ve learned not to take that for granted. I always talk about my ‘next treatment’—not because I’m obsessed with what might go wrong, but because it helps me feel prepared. Knowing what’s next gives me peace of mind. Even just the thought that I have a plan in place helps me sleep better at night. It doesn’t take the fear away, but it makes it feel manageable.
Social: Don’t Carry It Alone
This journey is heavy, and while some people have a gift for sharing their feelings, many do not. And that’s perfectly okay. You don’t have to lay bare every emotion to be supported. Sometimes, just asking someone to walk with you, sit with you, or be near you is enough.
Connecting with others going through the same thing—whether through a Facebook group, local support network, or online forum—can also lift the fog. There’s something powerful about talking to someone who truly gets it. On the flip side, spending time with loved ones outside the cancer bubble—doing something totally unrelated—can also give you space to breathe.
What’s one small thing you could do with someone you trust before or after a scan? A quick walk, a text check-in, a cozy coffee date? These moments may seem small, but they offer grounding and comfort during uncertain times.
If you’re looking for a safe, supportive space filled with people who truly understand what you’re going through, we invite you to join our new Facebook group. It’s a place to connect with fellow patients and caregivers, exchange insights, and find comfort in high-quality, compassionate content.
Emotional: Tend to Your Heart
Scanxiety doesn’t just affect your body—it deeply affects your emotions too. It can make you feel afraid, irritable, sad, or even numb. These feelings can be confusing, especially when they don’t seem to match the scan result. But they are normal and deserve attention.
Writing in a journal may help you express and understand your emotions. You don’t need to write every day, just enough to notice patterns or clear your thoughts. It’s a safe way to put your worries somewhere other than your chest.
Try to recognize your strength in going through this cycle again and again. You are not overthinking—you are reacting to something real and hard. And the fact that you keep showing up says so much about your courage.
If you follow a spiritual or religious path, you might find comfort in prayer, meditation, or quiet reflection. Even simple breathing exercises can bring some peace when your mind is racing.
Sometimes, the feelings become too big to manage alone. That’s when reaching out to a counselor, therapist, or oncology social worker can help. They’re trained to support you through exactly this kind of stress, and seeking their help is a smart, brave step—not a sign of weakness.
This list is by no means exhaustive. Everyone’s path through scanxiety is different. If you’ve discovered your own ways to cope or have moments, rituals, or ideas that help soothe the waiting, please share them with us in the comment below. Your voice might be exactly what someone else needs to hear.
In Closing
Scanxiety is not just a buzzword—it’s a real, valid experience. It doesn’t make you weak. It makes you human. Whether you’re the patient, the caregiver, or the quiet supporter on the sidelines, this emotional load is heavy. And yet, through stories, support, and strategies, you are not walking this road alone.
So the next time you feel that familiar ache of fear before a scan, take a breath. Let someone hold your hand. Remind yourself: you’ve faced hard days before—and you’re still here.