Navigating cancer care options can be overwhelming, especially when confronting terms like “palliative care” and “hospice.” With over 2 million new cancer cases expected to be diagnosed in the US in 2025, understanding these care approaches becomes critically important. While both palliative care and hospice focus on comfort and symptom management, they differ significantly in timing, goals, and patient eligibility. Importantly, research suggests that early palliative care can actually extend survival in some cases, contradicting the common misconception that it signifies the end of life. This comprehensive guide explores the key differences between these approaches and addresses concerns about long-term survival for stage 4 cancer patients receiving palliative care.

Understanding the Fundamental Differences
Definitions and Core Purposes
Palliative care is a specialized medical approach focused on providing relief from symptoms, pain, and stress of serious illness while improving quality of life. Unlike what many believe, palliative care is comfort care that can be provided with or without curative intent. This means patients can receive palliative care alongside treatments intended to cure their cancer.
Hospice care, while similar in its comfort-focused approach, is specifically for patients who are no longer pursuing curative treatment. It represents comfort care without curative intent, typically when a patient no longer has curative options or has chosen not to pursue treatment because the side effects outweigh the benefits.
Eligibility Requirements
The eligibility criteria for these two types of care differ significantly:
Hospice eligibility requires certification from two physicians that the patient has less than six months to live if the disease follows its usual course. In the US, this six-month prognosis requirement is largely due to Medicare’s hospice benefit parameters, which fund more than 90% of hospice care in the United States.
Palliative care eligibility has much less rigid guidelines. It can begin at the discretion of the physician and patient at any time and at any stage of illness, whether terminal or not. This flexibility allows for earlier intervention and integration with curative treatments.
Timing of Care Introduction
When care is introduced makes a substantial difference in patient outcomes. Palliative care can begin at diagnosis, during curative treatment, or during end-of-life care. In contrast, hospice typically begins when curative treatments are stopped, usually when life expectancy is six months or less.
The American Society of Clinical Oncology (ASCO) recommends early integration of palliative care for patients with Stage IV cancer, recognizing its benefits beyond end-of-life care. This recommendation is supported by research showing improved quality of life and potentially extended survival.
A Real-Life Story: Hope and Healing During Palliative Care
When Sarah, a 52-year-old mother of two, was diagnosed with stage 4 colorectal cancer, her world turned upside down. After several rounds of chemotherapy, her oncologist introduced the idea of palliative care. Like many, Sarah felt a wave of confusion and sadness. She worried that “palliative care” meant giving up hope for a cure—that it was the beginning of the end.
But her care team explained that palliative care wasn’t about stopping treatment; it was about adding an extra layer of support. The palliative care specialists helped manage her pain, nausea, and fatigue, making it possible for Sarah to stay strong through aggressive cancer treatments.
Over the next several months, Sarah’s treatment plan included a combination of targeted therapies, surgery, and radiation—all with curative intent. The palliative care team worked closely with her oncologists, ensuring that her symptoms were controlled and her quality of life remained as high as possible.
There were tough days, but Sarah never felt alone. The palliative care team helped her navigate emotional ups and downs, coordinated her appointments, and provided guidance for her family. This support made it possible for Sarah to complete her treatments without interruption.
A year later, after a final round of scans, Sarah’s oncologist delivered the words she had hardly dared to hope for: “No evidence of disease.” Sarah was in remission.
Sarah’s experience is a powerful reminder that palliative care is not the end of the road. For many patients, it is a bridge—helping them live better and, in some cases, supporting them all the way to recovery. Palliative care can be part of a curative journey, providing comfort, strength, and hope when it’s needed most.
Living with Stage 4 Cancer: Beyond the Terminal Diagnosis
Stage 4 Cancer Is Not Always Terminal
While stage 4 is the most severe stage of cancer with the highest risk of mortality, it is not always terminal. Metastatic cancer refers to cancer that has spread to distant areas of the body, but advances in treatment have enabled many patients to live for extended periods with good quality of life.
The prognosis for stage 4 cancer varies widely depending on the type of cancer, the extent of metastasis, individual factors like age and overall health, and response to treatment. Many patients live well beyond the six-month timeline often associated with hospice eligibility.
Palliative Care as a Support for Living with Advanced Cancer
For stage 4 cancer patients, palliative care can provide crucial support that enhances quality of life without requiring the discontinuation of treatment. This includes:
- Management of cancer-related symptoms like pain, nausea, fatigue, and shortness of breath
- Emotional and psychological support for patients and families
- Coordination between multiple healthcare providers
- Assistance with difficult treatment decisions
- Support for daily living activities
These interventions help patients maintain the best possible quality of life while living with advanced cancer, whether for months or years.
Making Informed Decisions About Care Options
When to Consider Palliative Care
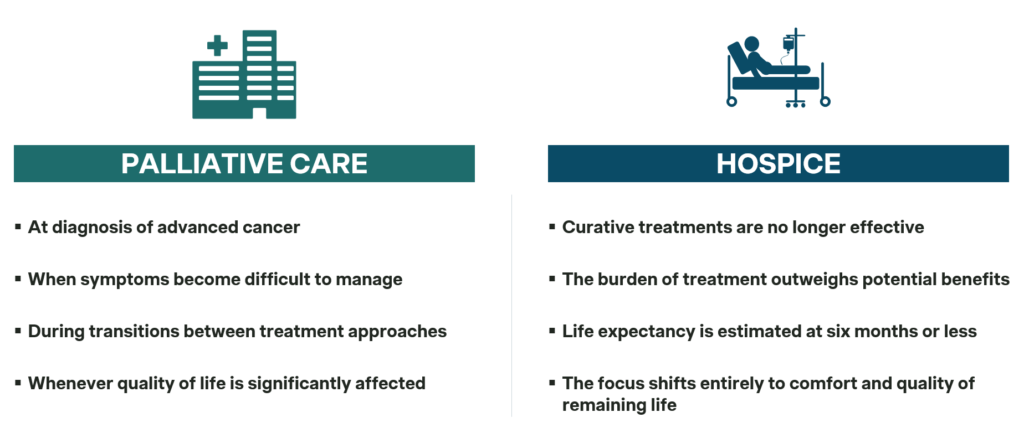
Palliative care should be considered early in the course of serious illness like cancer. Contrary to common belief, you don’t need to wait until the end stages of disease. Consider palliative care:
- At diagnosis of advanced cancer
- When symptoms become difficult to manage
- During transitions between treatment approaches
- Whenever quality of life is significantly affected
Early integration of palliative care with standard oncological care not only improves symptom management but may also extend survival.
When Hospice Becomes Appropriate
Hospice care becomes appropriate when:
- Curative treatments are no longer effective
- The burden of treatment outweighs potential benefits
- Life expectancy is estimated at six months or less
- The focus shifts entirely to comfort and quality of remaining life
The transition from palliative care to hospice isn’t always necessary—some patients receive palliative care until death without ever transitioning to hospice, especially if they continue pursuing disease-modifying treatments.
Conclusion
Understanding the differences between palliative care and hospice enables cancer patients and their families to make informed decisions about their care. The key takeaway is that palliative care is not exclusively end-of-life care—it can and should be integrated early in the disease trajectory, potentially alongside curative treatments.
For stage 4 cancer patients, palliative care offers a pathway to improved symptom management and quality of life without requiring the abandonment of hope or treatment. Research suggests that early palliative care may even extend survival in some cases, challenging the misconception that it hastens death.
As cancer care continues to evolve, the integration of palliative approaches throughout the cancer journey represents a more holistic model that addresses not just the disease, but the whole person living with cancer. By embracing palliative care early, patients with advanced cancer can focus on living well for as long as possible, rather than simply preparing for death.
Source: Canadian Oncology Nursing Journal; Asian Pacific Journal of Cancer Care; Pain Symptom Manage Journal; Vitas Healthcare.