Liver metastases represent a significant challenge in colorectal cancer (CRC) management, affecting approximately 20% of patients at initial diagnosis (synchronous) and up to 60% during disease progression (metachronous). This report synthesizes current treatment recommendations from major oncology organizations including ASCO, NCCN, and ESMO, highlighting evidence-based approaches based on disease presentation and therapeutic goals.
Classification of Colorectal Liver Metastases
The cornerstone of effective management begins with proper classification of liver metastases. Current guidelines universally recommend multidisciplinary team evaluation to categorize metastases into three distinct groups:
Resectable Disease
Characterized by limited liver burden with clear possibility for complete (R0) resection. Approximately 20-30% of patients present with initially resectable disease. ESMO guidelines specifically recommend upfront surgery for single liver metastases up to 2cm with favorable prognostic features. The treatment goal for this group is curative with potential for long-term survival.
Borderline/Potentially Resectable Disease
These patients have limited metastatic burden involving critical structures or insufficient future liver remnant (FLR). With appropriate preoperative strategies, conversion to resectable status is possible. Meticulous evaluation by hepatobiliary surgeons, medical oncologists, and interventional radiologists is essential for determining optimal approach.
Definitively Unresectable Disease
Patients with extensive liver metastases unlikely to achieve R0 resection despite optimal therapy. Treatment goals shift toward prolonging survival and maintaining quality of life, though cure is rarely achievable with conventional approaches.
Treatment Approaches for Resectable Liver Metastases
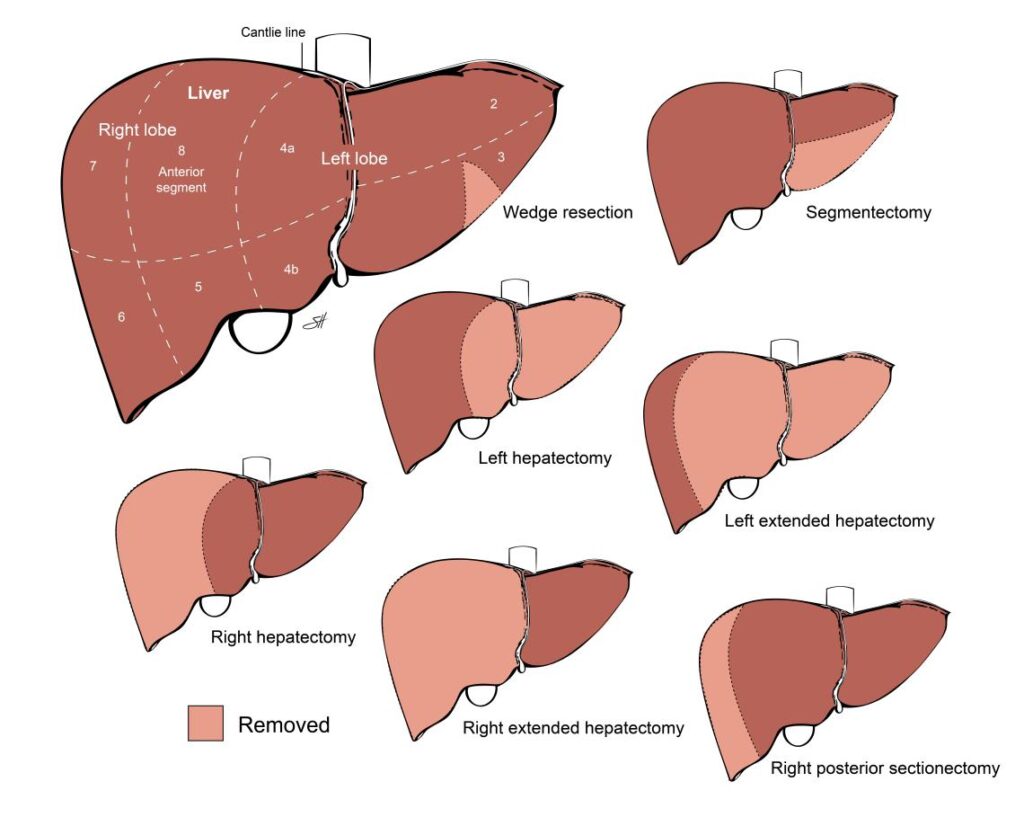
Surgical resection remains the gold standard for curative treatment of colorectal liver metastases (CRLM). Key recommendations include:
Surgical Options
For patients with clearly resectable disease, guidelines offer two primary pathways:
Upfront Surgery with Adjuvant Therapy: NCCN guidelines support immediate resection followed by adjuvant chemotherapy for appropriate candidates. This approach is particularly suitable for patients with limited disease and favorable biology.
Perioperative Chemotherapy: Both ASCO and ESMO guidelines endorse perioperative chemotherapy (preoperative followed by postoperative) for most patients with resectable disease, particularly for larger or multiple metastases. The EORTC 40983 trial demonstrated a 7.3% absolute improvement in progression-free survival with perioperative FOLFOX compared to surgery alone.
Surgical intervention demonstrates the best long-term outcomes, with 5-year overall survival rates reaching up to 58% in selected patients. The decision between these approaches should be individualized through multidisciplinary evaluation.
Management of Borderline/Potentially Resectable Disease
For patients with borderline resectable disease, conversion strategies are essential to achieve resectability:
Conversion Chemotherapy
Intensive preoperative systemic therapy is recommended to downsize tumor burden in borderline resectable CRLM. Both ASCO and NCCN guidelines recommend:
Doublet Chemotherapy: FOLFOX or FOLFIRI regimens are standard approaches.
Triplet Chemotherapy: More intensive FOLFOXIRI regimens may be considered for fit patients with more extensive disease requiring significant downsizing. Recent four-drug combinations have demonstrated response rates up to 80%, making them promising for conversion purposes.
Biological Agents: Addition of targeted therapy is guideline-recommended based on tumor sidedness and molecular profile. For left-sided RAS wild-type tumors, anti-EGFR therapy is preferred, while for right-sided tumors, anti-VEGF therapy is recommended.
After successful downsizing, reassessment for resection should be performed every 2-3 months to identify the optimal window for surgical intervention.
Management of Unresectable Liver Metastases
For patients with definitively unresectable disease, several evidence-based options exist:
Systemic Therapy
ASCO guidelines recommend doublet chemotherapy or triplet therapy for previously untreated, initially unresectable mCRC. Therapy selection should incorporate molecular and clinical factors:
MSI-High/dMMR Tumors: Pembrolizumab is recommended in the first-line setting.
BRAF V600E-Mutant mCRC: Encorafenib plus cetuximab is recommended after progression on at least one previous line of therapy.
RAS Wild-Type: Treatment recommendations differ by primary tumor location, such as chemotherapy with anti-EGFR therapy for left-sided and chemotherapy with anti-VEGF for right-sided
Locoregional Treatments
Several non-surgical local approaches show promise for unresectable disease:
Ablative Therapies: For smaller tumors (≤3cm, ≤3 in number), image-guided ablation with margins >10mm offers local tumor control comparable to hepatectomy. Ablation combined with systemic chemotherapy significantly improves survival compared to chemotherapy alone in unresectable disease.
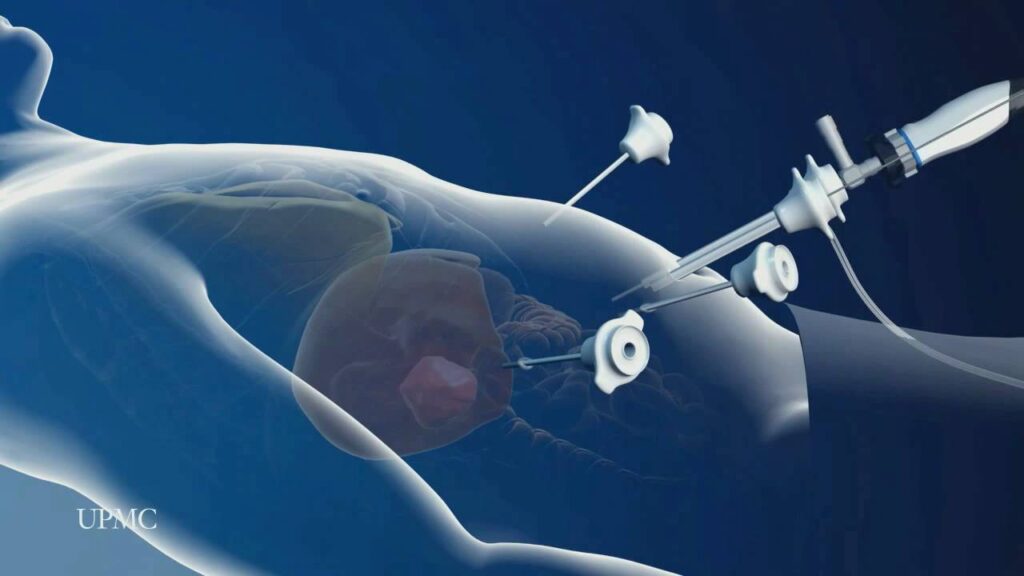
Stereotactic Body Radiation Therapy (SBRT): ASCO guidelines recommend SBRT following systemic therapy for patients with liver oligometastases not suitable for resection.
Regional Arterial Therapies: Various transarterial approaches exist, though routine use of selective internal radiation therapy is not recommended by ASCO for unilobar or bilobar metastases.
Liver Transplantation
The landmark TRANSMET trial recently presented at the 2024 ASCO Annual Meeting demonstrated significantly improved 5-year overall survival with liver transplantation plus chemotherapy (73%) versus chemotherapy alone (9%) for definitively unresectable CRLM. This represents a paradigm shift in the management of select patients with liver-limited, unresectable disease, with an 84% reduction in the risk of death in the per-protocol population.
Integrated Approaches for Complex Presentations
Several approaches blend multiple modalities for optimal outcomes:
Combined Modality Approaches
Surgery Plus Ablation: Hepatectomy combined with intraoperative or postoperative ablation can achieve local tumor control while preserving liver function in patients with extended disease distribution.
Cytoreductive Surgery Plus Chemotherapy: ASCO guidelines suggest this approach may benefit selected patients with colorectal peritoneal metastases, though hyperthermic intraperitoneal chemotherapy is not recommended.
Two-Stage Surgical Approaches
For patients with bilobar disease, staged resections may be employed to allow liver regeneration between procedures, potentially increasing the population eligible for curative-intent surgery.
Conclusion
Management of colorectal liver metastases requires individualized, multidisciplinary decision-making based on disease extent, patient factors, and molecular characteristics. Current guidelines from ASCO, NCCN, and ESMO provide complementary recommendations that can be summarized as:
Resectable Disease: Surgery (with or without perioperative chemotherapy) offers the best chance for cure, with 5-year survival rates exceeding 50% in selected patients.
Borderline Resectable: Intensive conversion chemotherapy followed by resection when possible provides meaningful survival benefit.
Definitively Unresectable: Systemic therapy remains the backbone of treatment, with growing evidence supporting ablative approaches, radiation therapy, and potentially liver transplantation in highly selected cases.
Regardless of presentation, guideline-based multidisciplinary management optimizes outcomes for patients with this challenging manifestation of colorectal cancer. Ongoing trials will further refine these approaches, particularly regarding the role of liver transplantation and novel combinations of local and systemic therapies.
NOTE: Individual results vary. Discuss your case with your care team. This guide synthesizes recommendations from leading oncology groups, including ASCO, NCCN, and ESMO


Como educador en salud valoro especialmente cómo sus artículos equilibran información técnica con consejos prácticos para el cuidado diario
Thanks for your kind comment. ¡Gracias!
Pingback: Stage IV Colon Cancer Survival: A Decade of Dramatic Improvement and Hope