Non-small cell lung cancer (NSCLC) is a complex and deadly disease, but recent advances in antibody-drug conjugates (ADCs) are offering new hope for patients. ADCs combine targeted precision with powerful cancer-killing drugs, making them a promising option for treating NSCLC. However, their path to success has been challenging, with setbacks and breakthroughs shaping the therapeutic landscape. This blog explores what ADCs are, why their development in NSCLC has been difficult, and highlights exciting progress in treatments for NSCLC.
What Are Antibody-Drug Conjugates (ADCs)?
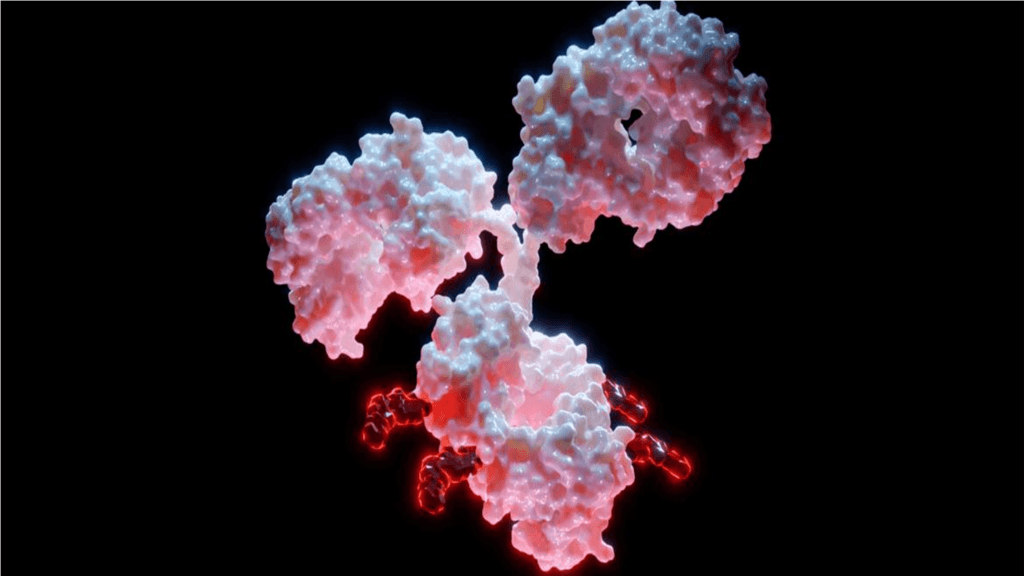
ADCs are an innovative type of cancer treatment that combines two key components:
- Antibodies: These proteins act like “smart missiles,” targeting specific markers (antigens) on cancer cells.
- Cancer-killing drugs: These highly potent drugs are delivered directly to the tumor to minimize harm to healthy tissues.
The antibody and drug are connected by a “linker,” which keeps the drug stable until it reaches the cancer cell. Once the ADC binds to the tumor, it enters the cell and releases its payload, killing the cancer from within. This targeted approach is designed to be more effective and less toxic than traditional chemotherapy.
Why Are ADCs Challenging in NSCLC?
Developing ADCs for NSCLC has proven difficult due to several factors:
Balancing Effectiveness and Safety
While ADCs are powerful, they can also cause serious side effects. NSCLC tumors vary widely in their biology, making it hard to predict which patients will respond well without experiencing severe toxicities like lung inflammation or damage to healthy tissues.
Tumor Complexity
NSCLC tumors are highly diverse—they don’t all express the same markers that ADCs target. This means an ADC might work well for some patients but not for others. Scientists are working on ways to better identify which patients will benefit most from these treatments.
Finding the Right Place in Treatment
With many options available for NSCLC—like immunotherapy and targeted therapies—it’s unclear where ADCs fit best. Should they be used after other treatments fail? Or should they be combined with other therapies? These questions remain open.
Learning From Setbacks: The Case of Tusamitamab Ravtansine
Not every ADC makes it to market successfully. One example is Sanofi’s tusamitamab ravtansine, which targeted a protein called CEACAM5 found on some NSCLC tumors. Despite showing promise early on, it didn’t perform well enough in a Phase 3 clinical trial to justify further development. The trial showed no significant improvement compared to standard chemotherapy, leading Sanofi to discontinue its program.
This failure highlights how difficult it is to turn scientific ideas into real-world treatments—especially in a disease as complex as NSCLC.
Recent Breakthroughs: Hope for advanced NSCLC
Despite challenges, two ADCs targeting TROP2 have made exciting progress for NSCLC patients, including those with EGFR mutations.
Sacituzumab Tirumotecan (Sac-TMT)
Sac-TMT recently gained approval in China for advanced NSCLC after resistance to prior therapies. It’s particularly noteworthy as the first TROP2-directed ADC approved for lung cancer globally. A phase 3 study is also ongoing in China, combining Sac-TMT with osimertinib for first-line treatment of locally advanced or metastatic NSCLC with EGFR mutations.
Sac-TMT uses a novel linker and payload design that allows it to kill tumor cells directly while also affecting neighboring cells through a “bystander effect.” This mechanism makes it particularly effective against tumors with diverse cell populations.
Datopotamab Deruxtecan (Dato-DXd)
Dato-DXd has shown promising results in various NSCLC populations, not just those with EGFR mutations. The phase 3 TROPION-Lung01 trial demonstrated significant improvement in progression-free survival compared to docetaxel in previously treated advanced or metastatic NSCLC patients, including both squamous and non-squamous histologies.
Key points about Dato-DXd:
- Efficacy was particularly strong in non-squamous NSCLC (about 75% of study population).
- The trial included patients with and without actionable genomic alterations.
- It showed a manageable safety profile with fewer dose reductions or discontinuations due to adverse events compared to docetaxel.
Dato-DXd features an advanced design with a tumor-selective linker and optimized drug-to-antibody ratio that aims to reduce side effects while enhancing efficacy.
How Are Sac-TMT and Dato-DXd Different?
Both Sac-TMT and Dato-DXd target TROP2 and show promise in NSCLC, including EGFR-mutated cases, but they have unique features:
- Sac-TMT: Approved first in China; focuses on delivering its payload directly into tumor cells while leveraging a strong bystander effect.
- Dato-DXd: Demonstrated efficacy in a broader NSCLC population; uses cutting-edge biomarker strategies and advanced linker technology to enhance precision targeting.
These differences may influence how doctors choose between them based on patient needs and treatment goals.
What’s Next for Patients?
The approval of Sac-TMT and the anticipated success of Dato-DXd signal exciting progress for patients with EGFR-mutated NSCLC—especially those who have run out of other options. However, these treatments aren’t without risks; side effects like lung inflammation need careful management by healthcare teams.
For caregivers and patients navigating treatment decisions, it’s important to ask your doctor about:
- Biomarker testing: Does your tumor express markers like TROP2 or EGFR mutations that make you eligible for these therapies?
- Side effect management: What steps can be taken to minimize risks during treatment?
- Combination strategies: Could an ADC work better alongside immunotherapy or other treatments?
Conclusion: A New Era for Lung Cancer Treatment
ADCs represent a bold step forward in lung cancer care—offering targeted precision that wasn’t possible with older therapies like chemotherapy alone. While challenges remain, recent approvals and trial results show that persistence pays off in developing these innovative drugs.
For patients and caregivers facing NSCLC, including those with EGFR mutations, these advancements bring hope that more effective options will continue to emerge. By working closely with healthcare providers and staying informed about new developments, you can explore cutting-edge treatments that may improve outcomes—and quality of life—for those battling this disease.
The future of antibody-drug conjugates is bright—and it’s paving the way toward better care for lung cancer patients everywhere!
Source: AstraZeneca Press Release (September 2024), OncLive (March 2025)


