Lung cancer remains one of the leading causes of cancer-related deaths around the globe. Among its various forms, non-small cell lung cancer (NSCLC) is by far the most common, making up about 80–85% of all lung cancer diagnoses. When it reaches an advanced stage—often referred to as Stage IV or metastatic NSCLC—the cancer has spread beyond the lung to other parts of the body. Historically, treatments like surgery and radiation have proven less effective at this advanced point. Chemotherapy, particularly platinum-based regimens, became the standard option for many years, offering modest survival gains but often at the cost of significant side effects.
Over the past decade, however, a new type of treatment has reshaped the outlook for patients with advanced NSCLC. This approach, commonly known as immunotherapy, harnesses the body’s own immune system to fight cancer cells more effectively. Immunotherapy medications can help the immune system detect and attack tumors while often sparing more of the healthy tissue. In many cases, these drugs produce longer-lasting responses than chemotherapy alone. Although not a cure, immunotherapy has extended the lives of countless patients, turning advanced NSCLC from a uniformly grim diagnosis into a more manageable condition for many. In this post, we will explore how immunotherapy works, how doctors use it in advanced NSCLC, which treatments are currently available, and what patients can expect regarding side effects, outcomes, and future developments.
Understanding Advanced NSCLC
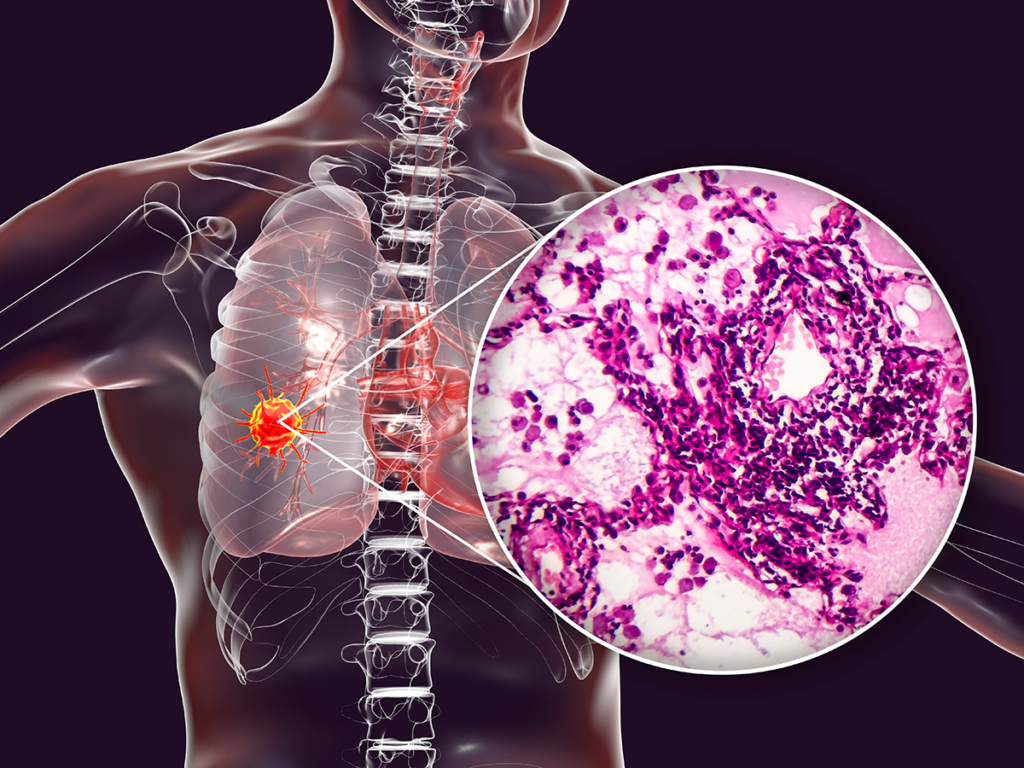
Non-small cell lung cancer (NSCLC) comprises several subtypes, the most common being adenocarcinoma, squamous cell carcinoma, and large cell carcinoma. Doctors use a staging system to determine how far the disease has spread. In Stage IV disease, also known as metastatic NSCLC, the cancer cells have traveled to distant sites—frequently the brain, bones, or liver. When patients reach Stage IV, their care team typically focuses on systemic treatments that address the body as a whole rather than localized interventions like surgery or radiation (though these can still be used in certain circumstances to manage specific issues).
Historically, advanced NSCLC care revolved around cytotoxic chemotherapy. A platinum-based agent such as carboplatin or cisplatin was usually paired with another chemotherapy drug. While many patients did see temporary tumor shrinkage or symptom relief, these gains often lasted only a few months, and chemotherapy sometimes caused severe nausea, fatigue, or low blood counts. Over time, researchers discovered that certain genetic alterations could be targeted with specific drugs. In patients with mutations in genes like EGFR or ALK, these new targeted therapies could be far more effective than chemotherapy alone. Still, the majority of patients did not have these mutations, leaving platinum-based regimens as their primary option.
The introduction of immunotherapy revolutionized this picture for many patients lacking “driver mutations.” By boosting a patient’s immune response, immunotherapy can lead to durable remissions that were once unimaginable. The unique side effect profile also distinguishes immunotherapy from older, more traditional regimens. Understanding how these drugs work can help patients and caregivers make informed decisions about their care.
How Immunotherapy Works in NSCLC
Under normal conditions, your immune system operates as a sort of surveillance network, identifying and eliminating abnormal cells—including cancer cells—before they can multiply uncontrollably. But tumors can develop strategies to hide from, or even suppress, the immune response. One key mechanism involves the proteins PD-1 (programmed death-1) and PD-L1 (programmed death ligand-1). PD-1 is located on the surface of T-cells, which are among the immune system’s most important cancer-fighting cells. PD-L1 is often found on tumor cells or surrounding immune cells. When PD-L1 attaches to PD-1, it sends a signal that effectively instructs the T-cells to stand down. This allows cancer cells to continue growing without being attacked.
Immunotherapy drugs known as immune checkpoint inhibitors block this interaction. Medications such as pembrolizumab (Keytruda), nivolumab (Opdivo), atezolizumab (Tecentriq), durvalumab (Imfinzi), and cemiplimab (Libtayo) target the PD-1 or PD-L1 pathway and prevent the tumor from evading detection. By releasing these “brakes” on T-cells, the body’s natural defenses become more capable of recognizing and destroying cancer cells. In certain NSCLC cases, this can lead to prolonged tumor control, sometimes lasting for years. Researchers are also exploring other checkpoints, such as CTLA-4, LAG-3, TIM-3, and TIGIT, in efforts to push immune cells even further against advanced lung tumors.
Immunotherapy in the First-Line Setting
When an individual is diagnosed with Stage IV NSCLC, one of the first questions for the oncologist is whether the cancer has specific biomarkers that might help guide therapy. Biomarker testing includes checking for gene mutations (EGFR, ALK, ROS1, among others) and also measuring PD-L1 expression. PD-L1 expression in the tumor can influence whether immunotherapy can be used alone or should be combined with chemotherapy.
Patients whose tumors show a high level of PD-L1 expression (commonly considered 50% or higher) may be offered immunotherapy alone. Pembrolizumab, for example, is often chosen for people with a “Tumor Proportion Score” (TPS) of at least 50%. This allows some individuals to avoid the side effects of chemotherapy. If the PD-L1 expression is lower, many oncologists recommend combining an immune checkpoint inhibitor with a platinum-based chemotherapy regimen. Studies reveal that chemo-immunotherapy combinations often produce better results than chemotherapy alone, even in patients whose tumors have minimal PD-L1 expression.
An example scenario might involve a 62-year-old diagnosed with Stage IV adenocarcinoma of the lung and a PD-L1 TPS of 60%. If no other actionable mutations are present, the oncologist might advise starting pembrolizumab alone. Another scenario could involve a 68-year-old with minimal PD-L1 expression, in which case the doctor could propose a combination of carboplatin, paclitaxel (or pemetrexed if non-squamous), and an immunotherapy agent such as pembrolizumab or atezolizumab. In both cases, the decision-making process also considers factors such as overall health, medical history, and the presence of other conditions like autoimmune diseases.
Patients who respond to immunotherapy in the first-line setting may stay on the drug for up to two years, provided they continue to benefit without unacceptable side effects. While not every patient will respond, the durability of tumor control is often more impressive than what doctors typically see with chemotherapy alone.
Second-Line and Beyond: Managing Resistance or Relapse
For many patients, initial treatments—whether immunotherapy or chemo-immunotherapy—eventually lose their effectiveness, and the cancer may start growing again. In earlier years, doctors might have turned to a second-line chemotherapy drug such as docetaxel. Today, they frequently offer an immune checkpoint inhibitor if a patient hasn’t already received one. Agents like nivolumab and atezolizumab can be considered in the second-line setting, showing improved survival compared to standard chemotherapy. Pembrolizumab might also be an option, especially for those whose tumors have notable PD-L1 expression.
If a patient has already used immunotherapy in the first-line setting, the next steps can be more complicated. Some patients transition to second-line chemotherapy, or they might explore trials testing new immunotherapy strategies or targeted agents. One essential consideration is whether the tumor harbors any genetic mutations that were not previously identified or that developed over time. Re-biopsies or liquid biopsy tests (which look for cancer DNA circulating in the blood) sometimes reveal mutations that open the door to targeted therapies not initially indicated.
Patients with EGFR mutations or ALK rearrangements typically start with specialized targeted drugs. If these targeted treatments eventually fail, immunotherapy might come into play, though data suggests that combining immunotherapy and EGFR inhibitors can elevate the risk of certain adverse reactions. The exact sequence of treatments is personalized, but the bottom line is that immunotherapy may serve as a critical lifeline for many advanced NSCLC patients who previously had few effective options once chemotherapy stopped working.
Managing Side Effects and Recognizing Immune-Related Toxicities
Although immunotherapy can be gentler than chemotherapy for many people, it creates a distinct set of side effects known as immune-related adverse events (irAEs). Because checkpoint inhibitors unleash the immune system, the body may inadvertently begin attacking healthy tissues. Problems can appear in various organs:
- Skin: Rashes or itching.
- Gut: Diarrhea, colitis (colon inflammation).
- Endocrine system: Hypothyroidism or hyperthyroidism, adrenal insufficiency, and, in rare instances, type 1 diabetes.
- Lungs: Pneumonitis (inflammation of lung tissue), which can be dangerous if not identified early.
- Liver: Hepatitis, usually discovered via elevated liver enzymes on blood tests.
Patients often receive detailed instructions on what to watch for. If you notice a persistent rash, new diarrhea, abdominal pain, unusual fatigue, breathing problems, or any other sudden health changes, it’s important to call your oncology team immediately. Prompt intervention can prevent a mild or moderate reaction from escalating into a severe one. Treatment for immune-related side effects typically involves temporarily pausing the immunotherapy and starting medications like corticosteroids to calm the immune system. In the majority of cases, these interventions are effective, especially if initiated promptly.
Education is a powerful tool here. Many cancer centers provide wallet cards or information sheets explaining the most common immunotherapy toxicities, emphasizing the need for urgent evaluation if something is amiss. Patients and caregivers should share this information with all their healthcare providers, including primary care doctors or emergency room staff, to help ensure that any new symptoms are evaluated in the context of immunotherapy.
Combining Immunotherapies with Other Treatments
Beyond the straightforward use of checkpoint inhibitors, doctors increasingly consider combination strategies that may produce stronger anti-cancer effects. One of the most common examples is chemo-immunotherapy. By pairing a platinum-based chemotherapy agent with an immunotherapy drug, it’s possible to reduce tumor burden quickly while simultaneously activating T-cells. Many pivotal trials demonstrate improved survival rates with these combinations compared to using chemotherapy alone.
Researchers are also exploring immunotherapy with anti-angiogenesis drugs (agents like bevacizumab that inhibit blood vessel growth in tumors). For instance, in certain types of non-squamous NSCLC, atezolizumab can be combined with bevacizumab and chemotherapy, leading to promising outcomes in some studies. Yet another approach involves “dual immunotherapy” that attacks more than one immune checkpoint at a time. For example, nivolumab (anti-PD-1) plus ipilimumab (anti-CTLA-4) has gained attention in advanced NSCLC, especially for patients with high tumor mutational burden. The goal is to unleash a more robust immune attack, although this approach can also increase the risk of more severe side effects.
Combination therapy, while often effective, must be balanced against potential toxicities. Patients should discuss with their oncologist whether the extra potency of dual or triple therapies is likely to outweigh the higher risk of immune-related problems. In some cases, a more “gentle” strategy may be preferred if the patient’s tumor shows certain characteristics, or if the patient has health issues that make them more vulnerable to serious side effects.
Looking Ahead: Ongoing Research and Clinical Trials
The field of immuno-oncology for NSCLC is evolving at a rapid pace, with numerous clinical trials seeking to refine existing treatments and discover new ones. Researchers are focusing on several main areas:
- Better Biomarkers: While PD-L1 expression guides some treatment decisions, it’s not always predictive of who will benefit. Studies are investigating tumor mutational burden (TMB), specific gene expression patterns, and other biological factors that might help determine the best therapy for each patient.
- Novel Immune Checkpoints and Combinations: Scientists are exploring drugs that target checkpoints beyond PD-1/PD-L1, such as LAG-3, TIM-3, and TIGIT. They also hope that pairing multiple immunotherapy agents might further improve patient outcomes.
- Personalized Vaccines and Cell Therapies: Some trials are testing therapeutic vaccines that train the immune system to attack tumor-specific antigens. Other research focuses on adoptive T-cell therapy, including CAR T-cells, which have transformed treatment for certain blood cancers but face additional challenges in solid tumors like lung cancer.
- Earlier-Stage Use of Immunotherapy: Immunotherapy is now being studied in locally advanced (Stage III) and even earlier stages of NSCLC, either before surgery (neoadjuvant therapy) or after surgery (adjuvant therapy) to reduce the risk of recurrence. Early results show improved survival and disease control in some settings, suggesting that harnessing the immune system early may prevent the cancer from re-establishing itself.
Patients interested in cutting-edge treatments should discuss the possibility of clinical trial enrollment with their care team. ClinicalTrials.gov maintains a comprehensive database of open and upcoming trials, offering a window into next-generation immunotherapy approaches.
Practical Guidance for Patients and Caregivers
Facing a diagnosis of Stage IV NSCLC can be daunting, and immunotherapy, while promising, can also raise questions about side effects and day-to-day management. Good communication with your oncology team is crucial to ensure you receive care tailored to your unique needs. You can help your doctors and nurses by keeping a log of any changes in your health, from skin rashes to fatigue, bowel movements, appetite, and breathing. Reporting issues early often helps keep problems manageable.
It is also important to ask about biomarker testing if it hasn’t already been done. While immunotherapy has helped many, some patients have genetic alterations (e.g., EGFR mutations) that respond better to targeted pills than to immunotherapy in the first-line setting. Knowing your tumor’s molecular profile can help the oncologist devise the most appropriate plan. Even if immunotherapy becomes your main treatment, staying on top of general health recommendations—such as quitting smoking, maintaining a balanced diet, staying active with short walks or gentle exercise, and addressing emotional health—is key. Many patients find counseling, support groups, or relaxation techniques beneficial, especially since the stress of a cancer diagnosis can impact mental well-being.
Caregivers play an equally critical role in encouraging patients to voice new concerns and providing daily practical support. Whether it’s coordinating transportation to appointments or helping track medication schedules, having a reliable network can make a huge difference in how smoothly treatment proceeds. Palliative care services can also be invaluable, even for those not yet facing end-of-life circumstances. Palliative care teams specialize in alleviating symptoms, managing side effects, and improving quality of life at any stage of a serious illness.
Conclusion: Finding Hope in Immunotherapy
A decade ago, advanced non-small cell lung cancer was often met with limited options: primarily chemotherapy, with modest results that rarely produced durable remissions. Immunotherapy has changed this landscape, allowing many patients to achieve longer survival times, deeper responses, and often fewer debilitating side effects than had been possible with chemotherapy alone. Although not every individual will respond to immunotherapy, and some may experience immune-related toxicities, the mere possibility of controlling metastatic lung cancer for months or years has profoundly shifted the attitudes of patients, doctors, and researchers alike.
As scientists delve deeper into understanding tumor biology and further optimize immunotherapy approaches, it’s likely we will see continued advancements in the management of advanced NSCLC. Already, the arrival of new biomarkers, novel immune targets, and more refined combination strategies promise even greater progress. For patients, the best path forward often involves open discussions with their oncology team about available therapies, potential clinical trials, and the overall goals of care—whether that be extending life, preserving quality of life, or balancing a bit of both.
If you or a loved one faces Stage IV NSCLC, know that you are not alone in this journey. Experts worldwide are dedicated to exploring innovative solutions, many of which are already delivering improved outcomes. By understanding the rationale behind immunotherapy, maintaining strong communication with your care team, and seeking supportive resources, you can navigate this challenging diagnosis with greater confidence and hope.
Sources and Further Reading
Disclaimer: This post is for educational purposes only and does not replace professional medical advice. Every patient’s health situation is unique, and treatment decisions should be made in consultation with a qualified oncology team. While immunotherapy offers new possibilities, it’s not a guaranteed solution for all. By staying informed and working closely with your doctors, you can find an approach best suited to your needs and goals.


