If you or a loved one has been diagnosed with stage IV (metastatic) colon cancer, it’s natural to feel overwhelmed. The diagnosis means the cancer has spread beyond the colon to other organs—most commonly the liver, lungs, or the lining of the abdominal cavity (peritoneum). While this is a serious and complex condition, treatment options are evolving rapidly, offering new possibilities for extended survival and, in some cases, even long-term remission.
Leading organizations like the American Society of Clinical Oncology (ASCO), the National Comprehensive Cancer Network (NCCN), and the European Society for Medical Oncology (ESMO) provide detailed guidelines for managing metastatic colon cancer. Although they may differ slightly in specific recommendations, all emphasize the importance of combination chemotherapy, targeted therapies guided by molecular profiling, and a team-based approach that can include surgery or local ablative treatments for certain metastases.
Below, you’ll find a comprehensive overview of the latest treatments for stage IV colon cancer, including when each approach is most effective, how to manage different metastatic sites (like liver or lung), and which new therapies are on the horizon. An Appendix at the end dives deeper into targeted therapies and immunotherapies, which now play a key role in managing metastatic colon cancer.
UNDERSTANDING STAGE IV COLON CANCER
Stage IV colon cancer means the disease has spread to distant organs or lymph nodes, well beyond the primary tumor in the colon. The liver is the most common site of spread, followed by the lungs, the peritoneum, and, less frequently, the bones. Although this diagnosis may feel overwhelming, it helps to know that treatment goals have evolved over the years. Doctors not only aim to prolong overall survival but also to preserve quality of life through effective symptom management. In certain cases—particularly when only a few metastases are present and can be removed—there may be a real opportunity for long-term remission or even a cure.
To craft the most effective treatment plan, physicians consider many factors: how widespread the disease is, whether the metastatic lesions can be surgically removed, and which genetic mutations or markers the tumor carries. Knowing details such as RAS/RAF mutation status, microsatellite instability (MSI), or HER2 amplification can be essential because these features help identify whether targeted therapies or immunotherapies might be beneficial. For instance, patients with RAS wild-type tumors might benefit from anti-EGFR therapies, whereas those with a BRAF V600E mutation might respond to a combination of encorafenib with an EGFR inhibitor. If the tumor is MSI-high (or mismatch repair deficient), immunotherapy may offer a particularly strong response.
Before diving into the different lines of treatment, it would be highly beneficial to first familiarize yourself with the following targeted therapies and immunotherapies, as they will play a crucial role in your cancer journey moving forward
Anti-EGFR Agents
Cetuximab (Erbitux) and Panitumumab (Vectibix) target the epidermal growth factor receptor (EGFR). This approach is most effective for tumors that do not have KRAS or NRAS mutations. Common side effects include skin rash, diarrhea, and fatigue.
Anti-VEGF Therapy
Bevacizumab (Avastin) works by inhibiting the vascular endothelial growth factor (VEGF), thereby cutting off the blood supply that tumors need to grow. It is commonly used in combination with various chemotherapy regimens. Side effects can include high blood pressure and bleeding risks.
BRAF Inhibitors
Encorafenib, often used alongside cetuximab or panitumumab, targets the BRAF V600E mutation. Combining a BRAF inhibitor with an EGFR inhibitor (and sometimes a MEK inhibitor in trials) can be more effective than using these agents alone.
HER2-Targeted Therapies
Trastuzumab and other HER2 inhibitors are used in certain cancers that overexpress the HER2 protein. In colon cancer, only a small percentage of tumors have this feature, but for those who do, HER2-targeted therapy can be a powerful tool.
Immunotherapy (Checkpoint Inhibitors)
Pembrolizumab, Nivolumab, and Ipilimumab are examples of checkpoint inhibitors. They help the immune system recognize and attack cancer cells more effectively. Their most remarkable benefits are seen in MSI-high or mismatch repair–deficient tumors. Because they rev up the immune system, they can cause inflammation in various organs (e.g., skin, colon, liver), which needs close medical monitoring.
If you’re finding these new terminology challenging, our cheatsheet provides a clear roadmap (See here).
FIRST-LINE THERAPIES
Most individuals with stage IV colon cancer begin treatment with combination chemotherapy. Common first-line regimens include FOLFOX (5-fluorouracil, leucovorin, and oxaliplatin), FOLFIRI (5-fluorouracil, leucovorin, and irinotecan), or CAPEOX (capecitabine and oxaliplatin). The choice often depends on the patient’s overall health, existing side effects or comorbidities, and personal preference (for instance, some may prefer oral capecitabine over continuous IV infusions). In certain situations—especially in younger or fit patients with a high burden of disease—a more intensive regimen known as FOLFOXIRI (5-FU, leucovorin, oxaliplatin, and irinotecan) may be considered.
Many patients also receive a targeted drug along with chemotherapy if their tumor’s genetics permit. Bevacizumab (Avastin), an anti-VEGF medication that blocks blood vessel formation, can be combined with any chemotherapy regimen. Anti-EGFR therapies like cetuximab or panitumumab may be used if the tumor is RAS wild-type (i.e., no RAS mutation). For tumors with high microsatellite instability, immunotherapy (pembrolizumab or similar checkpoint inhibitors) can sometimes be used right from the start, even without chemotherapy.
Using chemotherapy in combination with a biologic or immunotherapy can boost response rates, potentially shrink metastatic lesions enough to make them removable by surgery or local ablation, and in some cases extend survival by a significant margin.
SECOND- AND THIRD-LINE TREATMENTS
When cancer progresses despite first-line therapy, the next step often involves switching to a different chemotherapy regimen or adding a new targeted therapy, depending on what was used previously. If a patient began with an oxaliplatin-based regimen (like FOLFOX), doctors might switch to an irinotecan-based regimen (FOLFIRI) for second-line treatment, or vice versa. Sometimes targeted drugs, such as EGFR inhibitors or bevacizumab, can either be continued or introduced in later lines if they show benefit or were not used initially.
Other agents, such as regorafenib (a multikinase inhibitor) or trifluridine/tipiracil (Lonsurf), are approved for patients whose cancer has progressed after standard chemotherapy and available targeted therapies. These drugs can still help control the disease, although their side effects can be challenging. In some cases, doctors will order another biopsy (either from the tumor or via a “liquid biopsy” in the bloodstream) to look for newly emerged mutations that might guide further treatment or clinical trial eligibility.
LOCAL TREATMENTS FOR METASTASES
Not all patients with metastatic disease are candidates for surgery or local therapy, but there are important exceptions. When metastatic lesions are limited—often called “oligometastatic disease”—and located in places that surgeons or interventional radiologists can safely reach, local treatments can potentially lead to long-term control or remission.
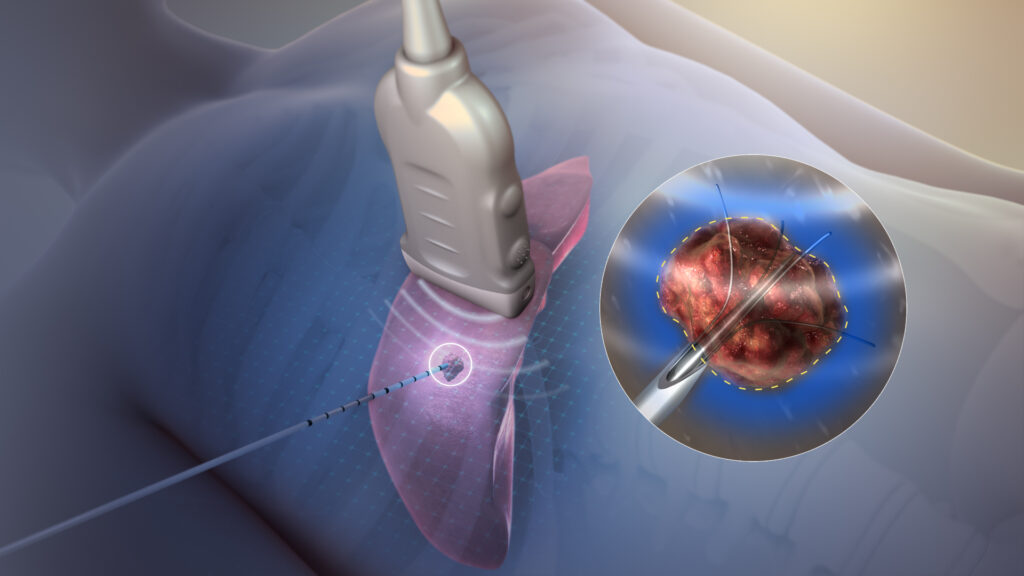
LIVER METASTASES: Resecting liver metastases, for example, can be very effective for patients who have only a few tumors confined to the liver. Ablation techniques (such as radiofrequency ablation or microwave ablation) may destroy small liver metastases without requiring major surgery, while techniques like Transarterial Chemoembolization (TACE) and Selective Internal Radiation Therapy (SIRT) target inoperable liver lesions.
LUNG METASTASES: Similarly, lung metastases can sometimes be surgically removed or treated with highly targeted radiation called Stereotactic Body Radiotherapy (SBRT).
PERITONEUM: For those whose disease has spread widely throughout the peritoneum, a combination of cytoreductive surgery and Hyperthermic Intraperitoneal Chemotherapy (HIPEC) may provide considerable benefit in select cases.
These procedures require a team of specialists—medical oncologists, surgical oncologists, interventional radiologists, and radiation oncologists—to evaluate each situation and collaborate on the best approach. Not everyone qualifies for these interventions, but for patients who do, the outcome can be significantly improved when combined with systemic treatments.
REAL-LIFE SCENARIOS
To illustrate these treatments in practice, the following patient cases may provide insights
In one example, a 50-year-old patient who has a primary colon tumor and two small metastases in the liver might start with a few months of FOLFOX chemotherapy combined with bevacizumab. If a scan shows the liver lesions have shrunk, a surgical oncologist might remove both the colon tumor and the liver metastases, followed by additional chemotherapy after surgery. This multi-step plan could result in long-term remission.
In a different scenario, a 60-year-old patient with widespread peritoneal metastases might begin with FOLFIRI and cetuximab, especially if testing shows a RAS wild-type tumor. If imaging later suggests that enough tumors have responded or shrunk, a specialized surgeon might consider cytoreductive surgery plus HIPEC, though that is only feasible for certain patients whose disease can be “debulked.” Otherwise, the patient might proceed to second-line treatments or explore clinical trials.
EMERGING TREATMENTS AND CLINICAL TRIALS
Colon cancer treatment is a rapidly evolving area of medicine, driven by ongoing research to find more effective and less toxic therapies. Clinical trials represent a key pathway for these innovations. Here are some of the promising avenues under investigation:
Researchers are exploring novel immunotherapy combinations, particularly for MSI-stable tumors that do not respond as robustly to single-agent checkpoint inhibitors. There is also intense interest in CAR T-cell therapies, which have seen success in certain blood cancers and are now being adapted for solid tumors like colon cancer. Bispecific T-cell engagers (BiTEs) are another exciting approach, designed to bring cancer cells and immune cells together to facilitate targeted tumor cell killing.
In addition to immunotherapies, drug developers are working on inhibitors for KRAS mutations—particularly KRAS G12C—and on improved therapies for patients who have BRAF or HER2 alterations. The gut microbiome is another emerging area, as scientists learn more about how gut bacteria may influence treatment efficacy and side effects.
If standard treatments stop working or if you meet specific eligibility criteria, joining a clinical trial can offer early access to these innovative therapies. Ask your healthcare team for guidance, or consult reputable databases such as ClinicalTrials.gov to learn more about ongoing trials in your region.
CONCLUSION
Metastatic colon cancer is a complex diagnosis that requires a comprehensive, individualized approach. Thanks to substantial advancements in chemotherapy, targeted therapies, immunotherapies, and surgical methods, many people are living longer and enjoying a better quality of life than ever before. In certain instances, a combination of chemotherapy and local treatment can even clear metastatic disease, leading to long-term remission.
If you or someone you care for is dealing with stage IV colon cancer, keep in mind that:
- Molecular profiling is important. Knowing whether the tumor is MSI-high, BRAF-mutated, HER2-positive, or has a specific RAS status can open doors to more personalized treatment.
- First-line therapy frequently involves chemotherapy plus a targeted drug or immunotherapy, depending on the tumor’s genetic features.
- Local treatments like surgery or ablation may be possible in some cases and can significantly impact outcomes.
- Clinical trials are vital to the future of colon cancer treatment and may present opportunities to try new approaches, especially when standard therapies have been maximized.
- A multidisciplinary care team—encompassing medical oncologists, surgeons, interventional radiologists, radiation oncologists, and supportive care providers—can tailor the plan to each individual situation.
Even though stage IV colon cancer remains a serious challenge, the landscape of care is rapidly evolving. Keep asking questions, seek supportive resources, and maintain open communication with your healthcare team. A combination of knowledge, teamwork, and the latest medical insights can pave the way to better outcomes and a fuller life.
SOURCES
- NCCN Guidelines for Colon Cancer
- ESMO Guidelines for Metastatic Colorectal Cancer
- ClinicalTrials.gov (for ongoing trials in metastatic colorectal cancer)
Disclaimer: This content is for educational purposes only and should not be taken as medical advice. Always consult a qualified healthcare professional for personalized treatment decisions.


